Melissa Do’s story begins not in a lab or a classroom, but across the Pacific a half century ago, rooted in the courage of her parents who fled war-torn Vietnam in search of a new life.
 Melissa Do Her mother fled in 1975, and a few years later, her father was rescued at sea by a U.S. naval ship after running out of food, having ensured every woman and child was safe before he left the boat himself. That act of selflessness would become a family legacy.
Melissa Do Her mother fled in 1975, and a few years later, her father was rescued at sea by a U.S. naval ship after running out of food, having ensured every woman and child was safe before he left the boat himself. That act of selflessness would become a family legacy.
“He stayed with the captain’s family, helped around their home and eventually got into college,” Do recalls. “My parents came from nothing, but gave everything.”
Do grew up in Huntsville, Alabama, where her parents worked in missile defense, serving over three decades to the Department of Defense. Engineering was the family language.
“They were my role models – so smart, so humble. I was obsessed with my parents growing up,” she said.
Engineering seemed like the natural path, but it was a visit to Vietnam as a teenager that shifted her direction.
“I saw firsthand the lack of access to healthcare and how limited resources affected people’s well-being. I wanted to do something that merged science and service.”
That calling led her to the University of Alabama at Birmingham, where she pursued biomedical engineering and eventually entered the neuroengineering Ph.D. program. Now a candidate nearing her dissertation defense, Do is conducting pioneering research in non-pharmaceutical interventions for sleep disorders among breast cancer patients.
At the heart of this work is transauricular vagus nerve stimulation – a gentle, non-invasive electrical stimulation technique applied through the ear to modulate the body’s stress response and improve sleep.
“Sleep is so foundational to healing,” Do explained. “These women are going through hormone therapy, chemo or radiation and they’re still being mothers, working jobs. It's amazing, but the stress and physical toll disrupt their sleep, which slows their recovery.”
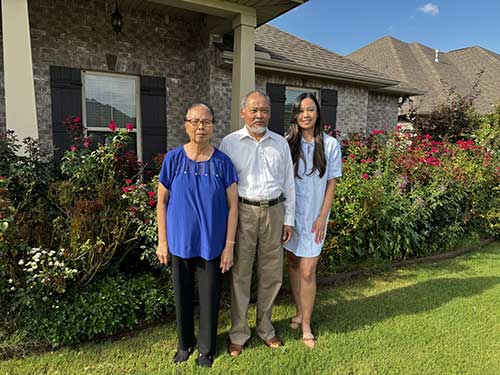 Melissa Do with her parents on her father's birthdayHer research, funded by the Palliative Research Enhancement Project (PREP), aims to offer a safe, accessible alternative to sleep medications – many of which breast cancer patients are reluctant to use due to side effects and drug fatigue.
Melissa Do with her parents on her father's birthdayHer research, funded by the Palliative Research Enhancement Project (PREP), aims to offer a safe, accessible alternative to sleep medications – many of which breast cancer patients are reluctant to use due to side effects and drug fatigue.
“One participant texted me a few days in and said, ‘I slept so good. My grandkids were running around, and instead of yelling at them, I was just laughing,’” Do said with a laugh of her own. “That was huge. She was skeptical at first. But that’s the real impact.”
That impact wouldn’t be possible, she adds, without the support of CEDHARS and the Adaptive Human Performance Lab, the facility where she runs her pilot study.
“It’s been such a privilege,” she said. “The infrastructure, the mentorship, even the environment – people peek their heads in because the space is so welcoming. Every time I walk down the hall, I’m reminded this is where academia and science meet compassion. It’s not just research – it’s about people.”
Participants, too, have felt that sense of connection.
“They often say it doesn’t feel like a doctor’s office – it feels personal. They feel heard. I think that’s why we haven’t had any dropouts in the study.”
Beyond the lab, Do is keenly aware of the broader implications of her work.
“We hope this becomes a foundation for non-invasive treatments that improve sleep, mood and inflammation – not just for breast cancer patients, but for everyone. Sleep disorders are so common and so overlooked, yet they impact every part of our lives.”
For Do, the intersection of empathy, science and innovation is where she finds purpose.
“Engineering gave me the tools. But empathy – my parents, the women in my study, the mentors I’ve had – gave me the reason. That’s what keeps me going.”
At the core of her work and drive, though, is the recognition of the impact of her roots. From the trans-Pacific journey to the take-your-kid-to-work days, where Do grew a fascination with technology, she can’t emphasize enough the guiding light her parents have been.
“They’ve been my why. They made incredible sacrifices and built a life here so that I could have opportunities like this. They’re retired now and traveling the world. I tell them all the time they should write a book.”

