As flowers bloom and temperatures climb, spring brings in allergy season for many. When sneezing, itchy eyes or sinus pressure strikes, knowing whether to see a general allergist or an ENT (ear, nose and throat) allergist can be confusing.
When to see an ENT allergist
General allergists specialize in a wide range of allergic and immune system disorders, addressing conditions beyond the ENT area, such as seasonal allergies, food allergies, asthma, anaphylaxis, hives, eczema and immunodeficiency disorders.
“In contrast, ENT allergists focus on allergies affecting the ears, nose and throat,” said Edwyn Boyd, M.D., clinical professor in the UAB Department of Otolaryngology.
They treat conditions like sinusitis, hay fever (allergic rhinitis), allergic conjunctivitis and other ENT-related allergy problems.
If over-the-counter medications provide only minimal relief, it may be time to consult an ENT allergist. These specialists can provide targeted care, especially for patients with chronic ENT issues linked to allergies.
“Recent advances, like injectable biologics, have shown promising results for severe or persistent cases, particularly for patients with chronic sinusitis and nasal polyps driven by allergies,” Boyd said.
Allergy or sinus infection?
Nasal congestion and facial pressure are common symptoms of both allergies and sinus infections, making it sometimes difficult to tell them apart. That is why an accurate diagnosis from an ENT allergist is needed for proper treatment.
“A thorough history of symptoms and a physical examination are essential for diagnosing both sinusitis and allergies,” Boyd said. “Sinusitis is a clinical condition that underlying allergies can trigger. While not all patients with sinusitis have allergies, and not all allergy sufferers develop sinusitis, many experience both conditions simultaneously.”
 A physical exam may reveal signs in allergic patients such as an “allergic” nasal crease, redness in the eye conjunctiva, allergic “shiners” (dark circles under the eyes), clear, watery nasal discharge, pale nasal mucosa and turbinate hypertrophy. In contrast, sinus sufferers may present with red, inflamed nasal mucosa, purulent discharge, nasal polyps and turbinate hypertrophy, without the typical allergy-related signs.
A physical exam may reveal signs in allergic patients such as an “allergic” nasal crease, redness in the eye conjunctiva, allergic “shiners” (dark circles under the eyes), clear, watery nasal discharge, pale nasal mucosa and turbinate hypertrophy. In contrast, sinus sufferers may present with red, inflamed nasal mucosa, purulent discharge, nasal polyps and turbinate hypertrophy, without the typical allergy-related signs.
Diagnosis and treatment options
In order to confirm allergies in patients, ENT allergists may use skin prick testing, intradermal testing, a combination of skin testing and intradermal testing, or blood tests. Skin testing is preferred for its sensitivity, while blood tests are more specific.
“For patients who experience symptoms in only one season, over-the-counter medications are typically the first line of treatment,” Boyd said. “Personally, I begin with an intranasal steroid spray as monotherapy and follow up with the patient to see if the medication has relieved the symptoms. If there’s only ‘some’ relief, I would then add a non-sedating oral antihistamine.”
Lifestyle and prevention
Avoidance is the most effective way to manage allergies, but it is often easier said than done.
“Pollen counts will be higher on hot, dry, windy days and greatest in the morning between 7 and 11 a.m.,” Boyd said. “To minimize exposure indoors, keep windows and doors closed, seal any drafts, and use air conditioning when possible. In enclosed workspaces, HEPA filters can help improve air quality when chosen based on room size.”
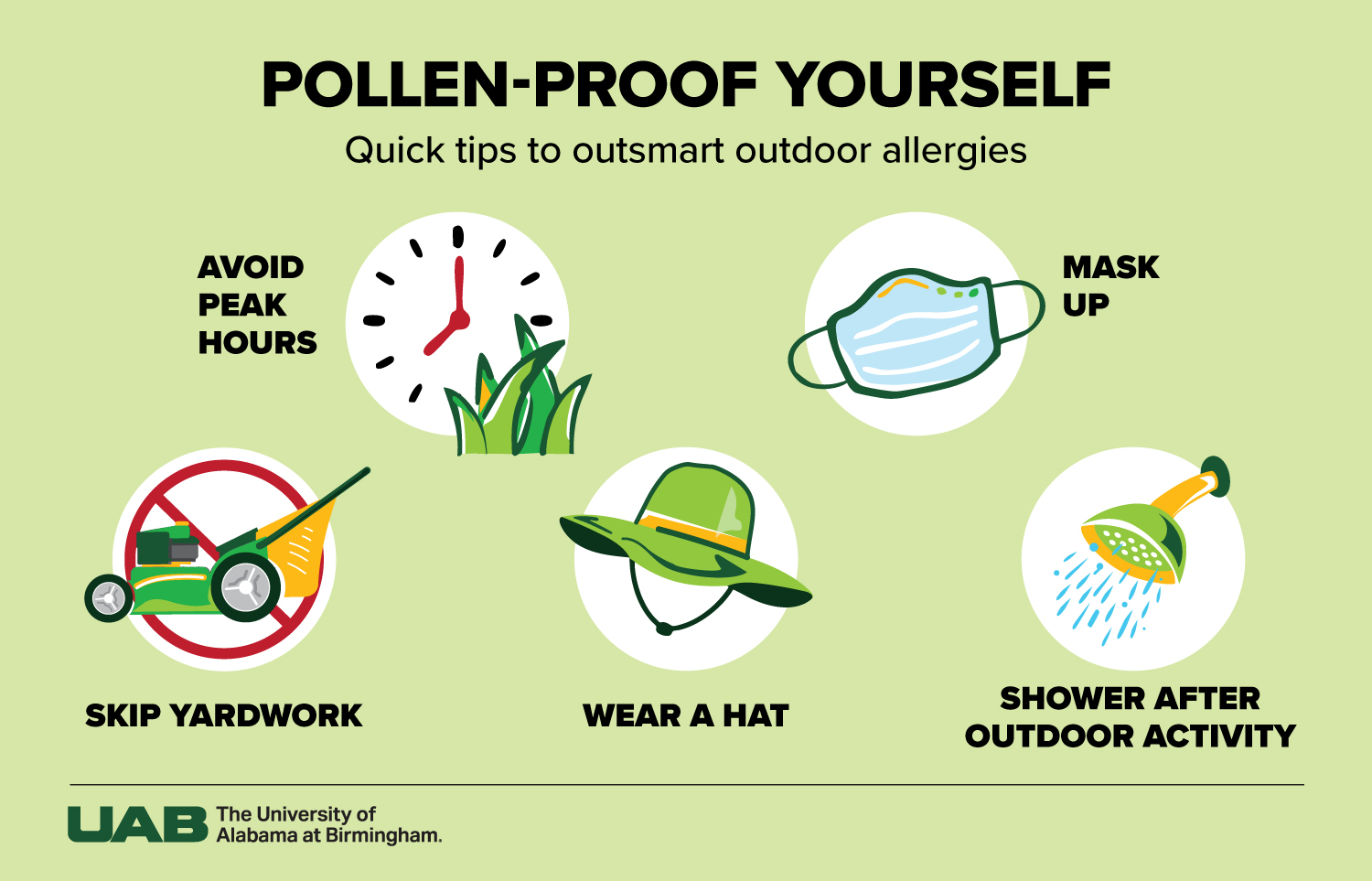
For outdoor pollen control, you should avoid yardwork, avoid outdoor activity (especially during peak hours), wear a hat, wear masks and shower after outdoor activity.