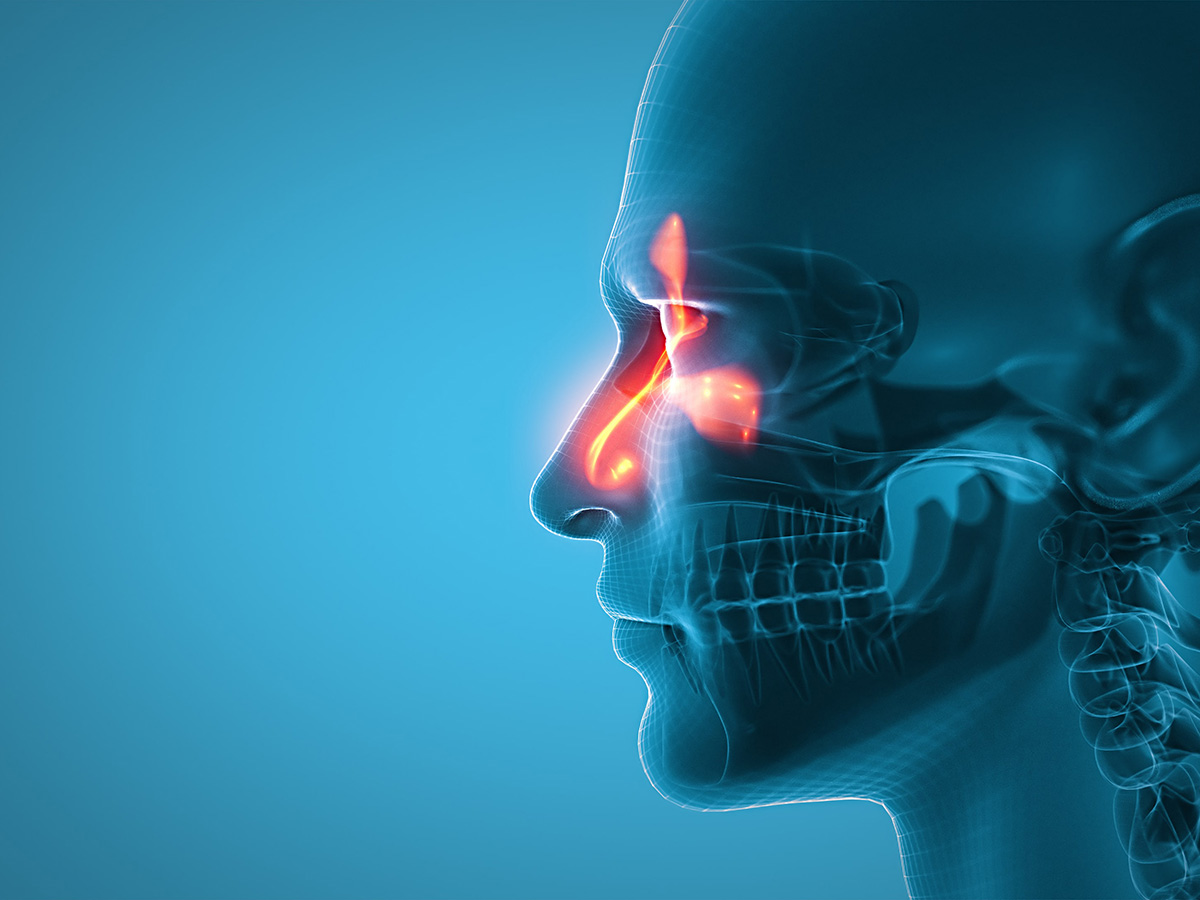
 A rare fungal sinus infection that used to affect mostly people in tropical countries is now showing up in the Southeastern United States, and doctors are learning how to better recognize and treat it thanks to new research from UAB.Chronic granulomatous fungal sinusitis is a rare, debilitating infection characterized by an enlarged mass in the nasal cavity or sinuses, facial pain and swelling, eye bulging, vision problems, headache, and nasal congestion. While most cases are found in subtropical regions of Sudan, India, Pakistan and Saudi Arabia caused by Aspergillus flavus, a pathogenic fungus, cases have recently been identified in the Southeastern United States caused by Curvularia, an emerging pathogen.
A rare fungal sinus infection that used to affect mostly people in tropical countries is now showing up in the Southeastern United States, and doctors are learning how to better recognize and treat it thanks to new research from UAB.Chronic granulomatous fungal sinusitis is a rare, debilitating infection characterized by an enlarged mass in the nasal cavity or sinuses, facial pain and swelling, eye bulging, vision problems, headache, and nasal congestion. While most cases are found in subtropical regions of Sudan, India, Pakistan and Saudi Arabia caused by Aspergillus flavus, a pathogenic fungus, cases have recently been identified in the Southeastern United States caused by Curvularia, an emerging pathogen.
Researchers from the University of Alabama at Birmingham published work in Modern Pathology highlighting six cases of chronic granulomatous fungal sinusitis. The article, titled “Histopathologic Insights into Curvularia-Induced Chronic Granulomatous Fungal Sinusitis: A Guide for Surgical Pathologists,” outlines findings from case examination to accurately update and guide future diagnosis and treatment of this infection.
“Surgical pathologists have to be aware of this infection’s expanded geographic range, affected populations and key histopathologic features,” said Ashleigh Riegler, Ph.D., a clinical microbiology fellow in the Department of Pathology and first author of the study.
While fungal sinusitis can be both noninvasive and invasive, chronic granulomatous fungal sinusitis is an invasive infection that is associated with slow progression of persistent nasal obstruction, discharge, facial pain and deformity, with potential extension into the orbital cavity and cranium. It can cause significant tissue destruction and require prompt diagnosis and treatment.
“In our histopathological examination, we found giant cells, granulomatous inflammation, short septate hyphae and segmented fungal filaments, with bulbous swelling,” said Sixto Leal, M.D., Ph.D., Jay M. McDonald Endowed Professor in Experimental Pathology, Division Director, Laboratory Medicine. “However, there was significant variation in size, shape and color, with half the cases lacking hyphal pigmentation and intracellular contents, yielding a characteristic ‘ghost shell’ morphology, indicating fungal nonviability.”
“Lack of awareness of this infection’s new variations led to initial misidentification of three cases,” said collaborator Peter Pappas, M.D., a professor in the UAB Department of Medicine’s . “It’s essential we know how to identify the emerging features of this infection.”
Riegler, Leal and Pappas, alongside their research team, found that Curvularia predominantly affects healthy African American men in the humid regions of the Southeastern United States. Treatment for this infection includes endoscopic surgery or a long-term antifungal medication treatment plan.
“We’re hopeful that the key features described in our case study will guide and equip surgical pathologists to accurately diagnose this rare emerging infectious disease in our area,” Riegler said.
Collaborators alongside Riegler, Leal and Pappas in this study include Jessica Grayson, M.D., Jacob Greenway, M.D., and Bradford Woodworth, M.D., UAB Department of Otolaryngology; and Todd McCarty, M.D., UAB Department of Medicine, Division of Infectious Diseases.