Case History:
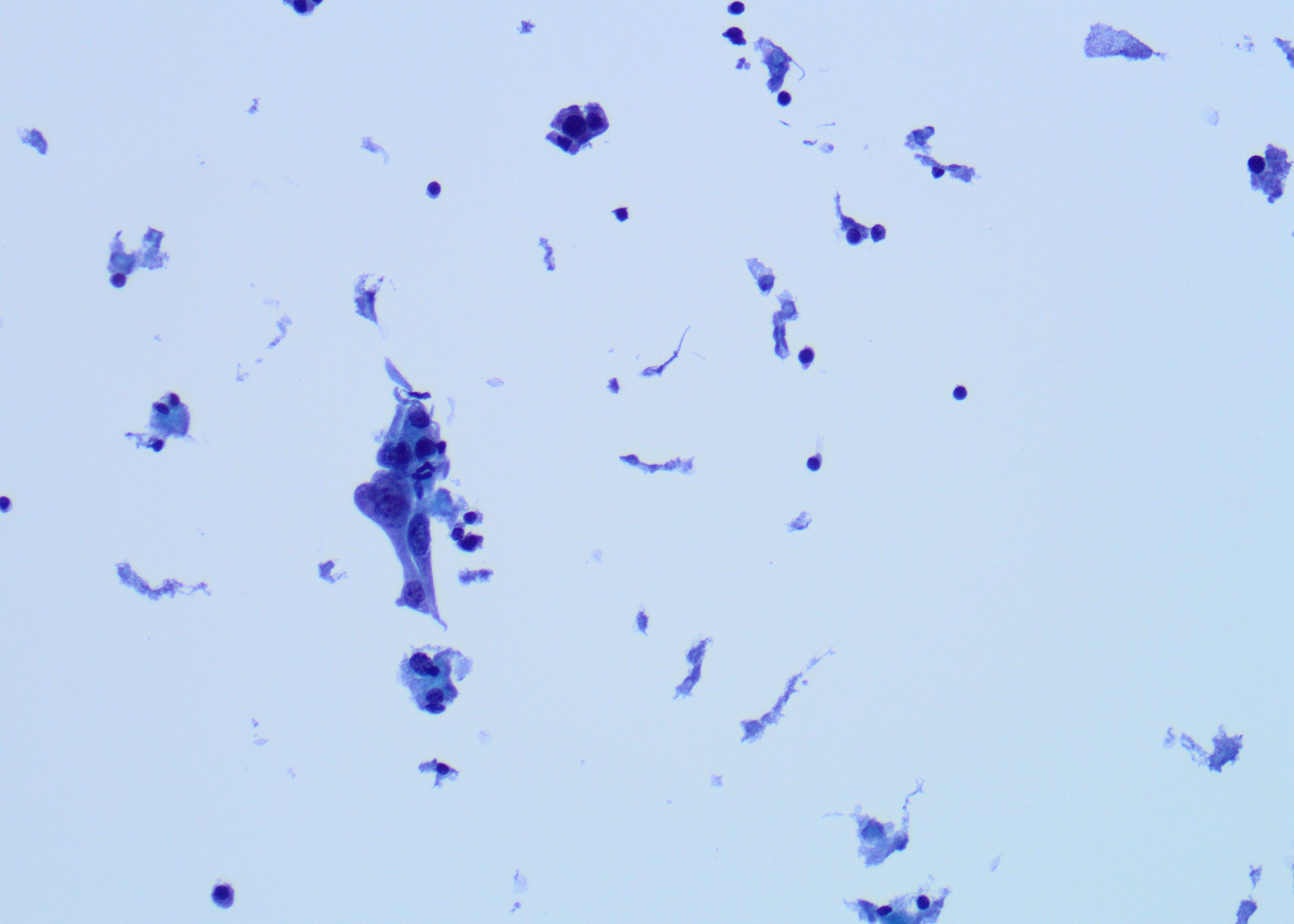
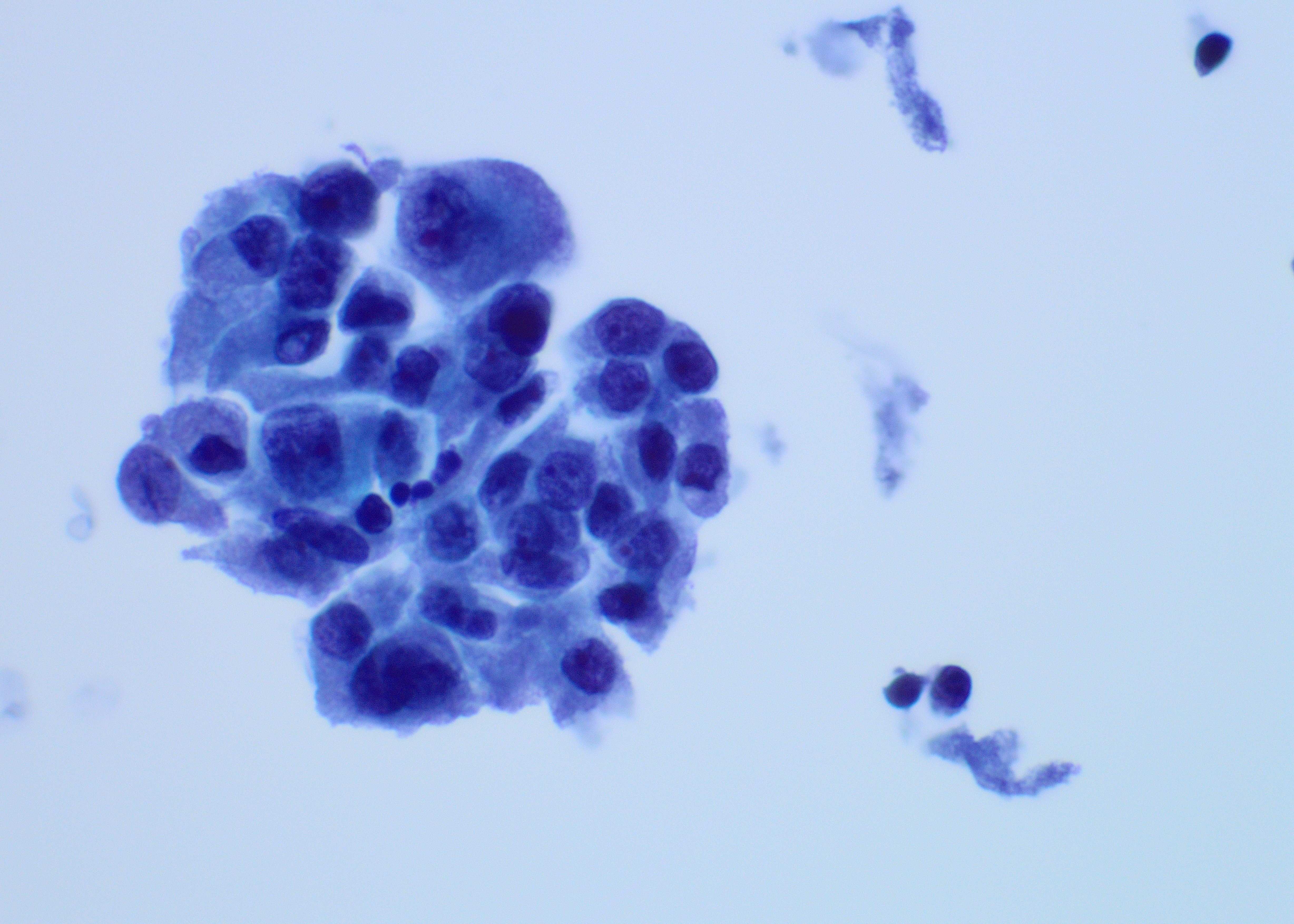
A 45-year old man with a history of PTC, tall cell variant (PT3b N1a M0), s/p total thyroidectomy, central neck lymph node excision and radioactive iodine therapy, presents with new neck mass. Figures a & b show FNA of the mass.
What is the most appropriate diagnosis?
A. Reactive/inflammatory process
B. Post radiation affect
C. Recurrent/metastatic thyroid carcinoma
D. Metastasis from an organ other than thyroid
Correct Answer: C. Recurrent/metastatic thyroid carcinoma
Discussion:
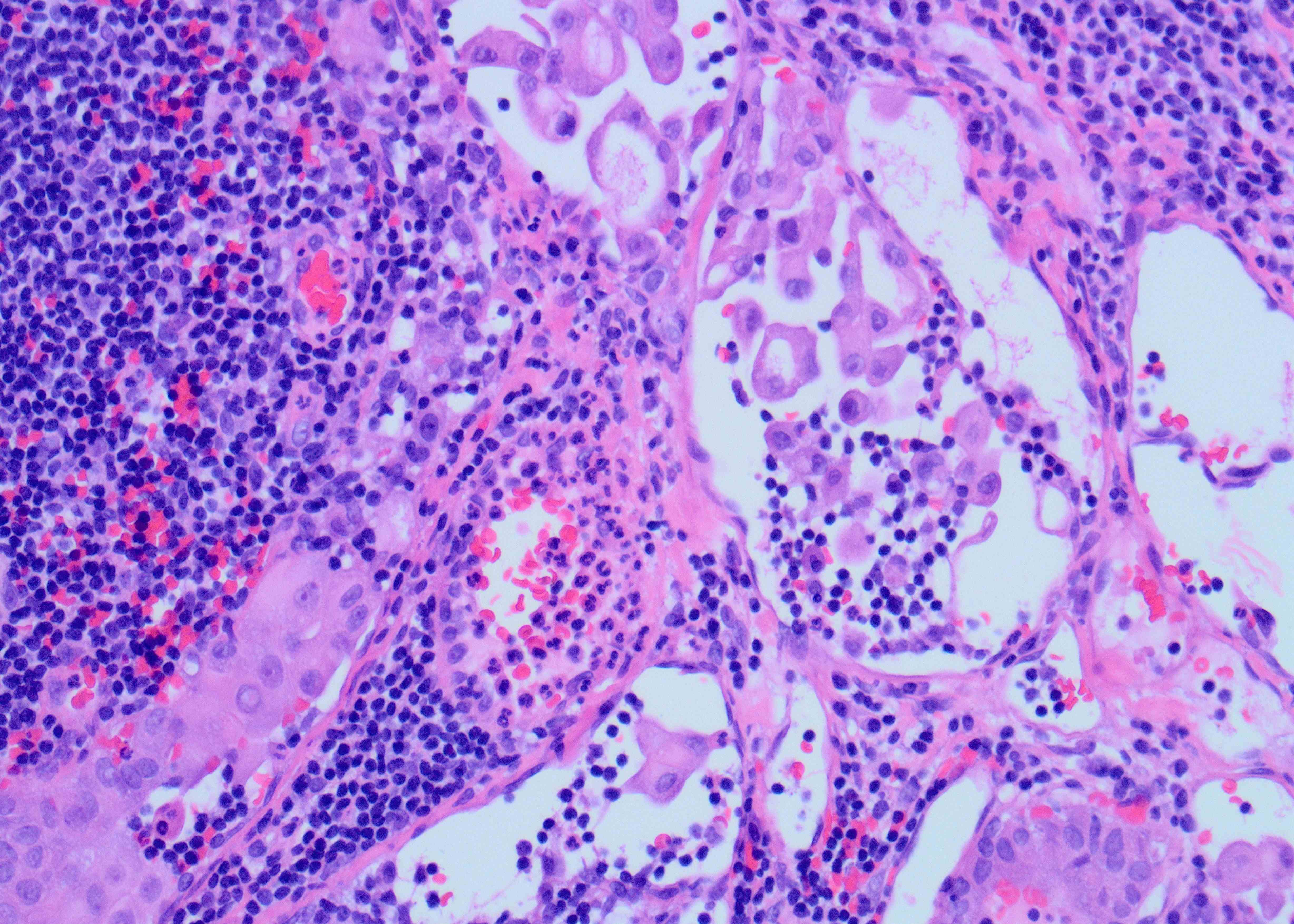
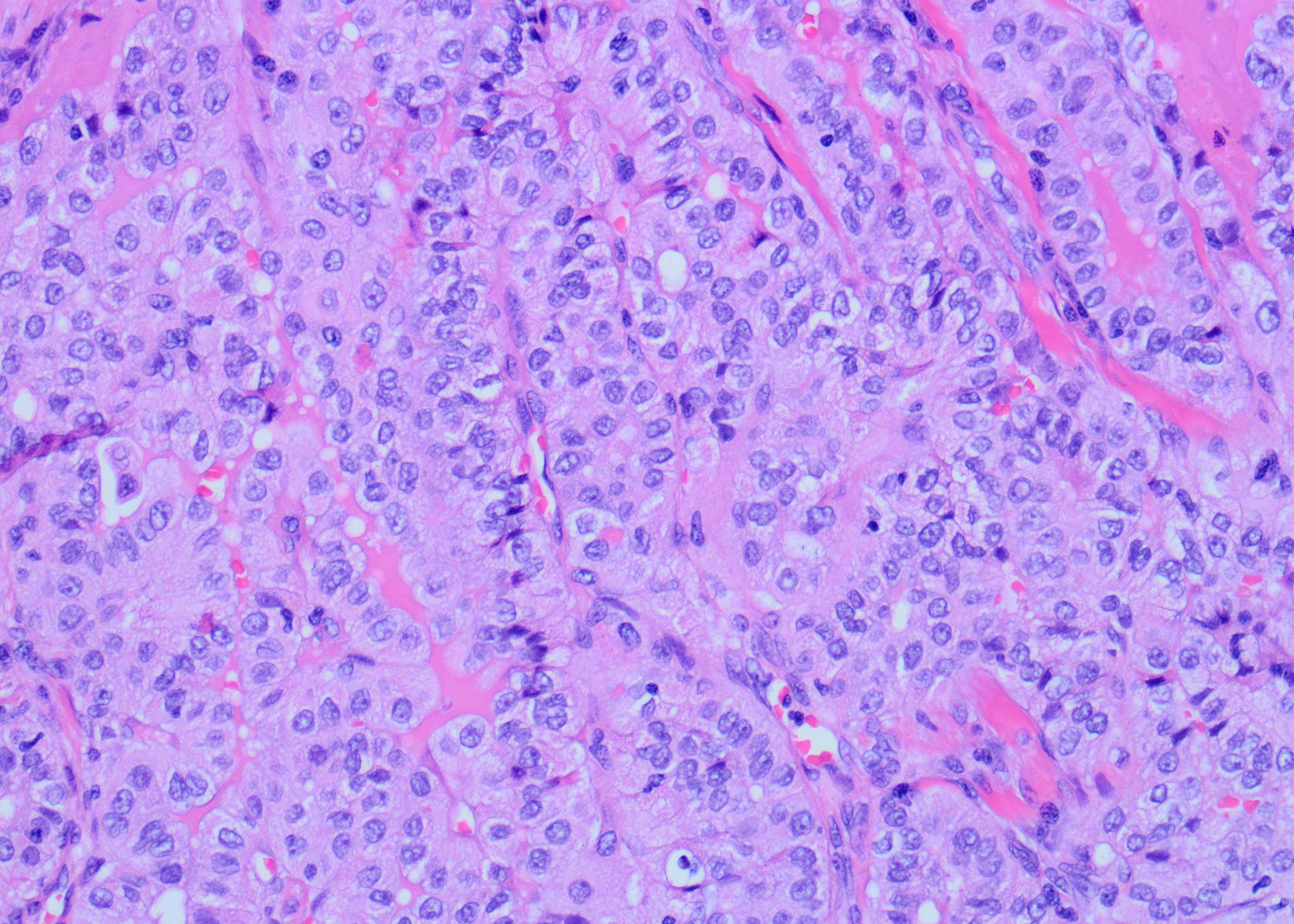
Although the specimen source was described as a neck mass, the presence of scattered lymphocytes in the back ground is suggestive of a lymph node aspirate. In addition, there are scattered clusters of large epithelioid cells but with relatively low nuclear to cytoplasmic ratio due to moderate amount of cytoplasm showing tapered cytoplasmic tails (Figure A). The high power shows a syncytial aggregate of atypical cells (Figure B). These cells have moderately abundant amount of granular cytoplasm with distinct margins. Occasional cells have tall cell morphology, evident predominantly along the periphery of the cluster as well as a single cell with soap bubble like intranuclear pseudoinclusion (arrow). The cytomorphology is identical to the metastatic cells present in the previously excised cervical lymph node (Figure C). All these features favor tall cell variant of papillary thyroid carcinoma (PTC), metastatic possibly to a cervical lymph node. Histopathologic feature of primary PTC, tall cell variant, is shown in Figure D.
Although cytoplasmic processes impart a tissue culture like appearance and raises the possibility of a post-surgical reparative process, like reactive fibroblasts, certain points argue against it, e.g., clinical presentation as a neck mass, presence of cellular aggregates and nuclear pleomorphism, as well as epithelioid cells in a lymphoid background that always raises the possibility of metastatic process until proven otherwise. The patient had radioactive iodine post- surgical excision but never had radiotherapy to explain the changes, as radioactive iodine does not cause radiotherapy like affect. Finally, the cytomorphologic features are characteristic of tall cell variant of PTC and in this clinical setting metastasis from non-thyroidal organ will be unlikely.
PTC is the most common malignancy of the thyroid gland and has overall a favorable prognosis, with few exceptions like PTC, tall cell variant. This variant of PTC is often associated with more aggressive behavior with a higher risk of recurrence than classic PTC. Therefore, a preoperative diagnosis of tall cell variant or even noting the tall cell features on FNA may help in triaging for appropriate patient management. The most helpful cytologic diagnostic features include increased numbers of tall tumor cells arranged as single cells and at the periphery of cellular groups containing granular cytoplasm and distinct cell borders, cytoplasmic tails, and cytoplasmic cuffs (peripheral rimming of cytoplasm in cellular groups). Intranuclear “soap-bubble” pseudoinclusion is not readily identifiable but when present is specific for tall cell variant/ changes.
References:
Baum JE, Soong L, Scognamiglio T, Margolskee EM, Hoda RS, Rao R. Cytological diagnosis of papillary thyroid carcinoma with tall cells on ThinPrep liquid-based cytology. Diagn Cytopathol. 2019 Jun;47(6):541-546. doi: 10.1002/dc.24146. Epub 2019 Jan 16. PMID: 30648353.
Tanaka A, Hirokawa M, Higuchi M, Suzuki A, Yamao N, Hayashi T, Kuma S, Miyauchi A. Diagnostic clues indicating tall cell variants of papillary thyroid carcinoma in fine needle aspiration. Diagn Cytopathol. 2019 May;47(5):452-457. doi: 10.1002/dc.24122. Epub 2018 Dec 23. PMID: 30582297; PMCID: PMC6590126.
Case contributed by: Huma Fatima, M.D., Renal Section Head, Associate Professor, Anatomic Pathology