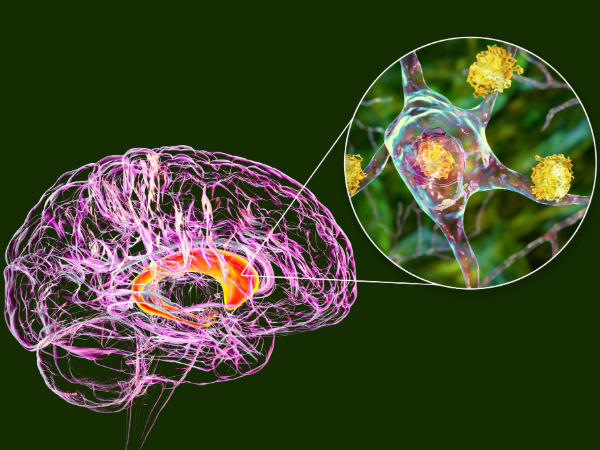
 A new treatment that proves to slow the progression of Huntington’s disease (HD) marks a breakthrough for a condition that has long been considered untreatable. Huntington’s is a rare, inherited neurodegenerative disorder that gradually deteriorates a person’s physical and mental abilities, often leading to death within 10 to 30 years of onset. Until now, treatments have only managed symptoms, rather than altering the disease’s course.
A new treatment that proves to slow the progression of Huntington’s disease (HD) marks a breakthrough for a condition that has long been considered untreatable. Huntington’s is a rare, inherited neurodegenerative disorder that gradually deteriorates a person’s physical and mental abilities, often leading to death within 10 to 30 years of onset. Until now, treatments have only managed symptoms, rather than altering the disease’s course.
Victor Sung, M.D., director of the Division of Movement Disorders in the UAB Department of Neurology and director of the UAB Huntington’s Disease Clinic, reacted to the initial results of the small clinical trial, which were released by the new therapy’s developer, uniQure, in late September.
“Since the HD gene was first sequenced over 30 years ago, we have been on a quest to try to slow or stop this difficult disease, and these preliminary results are finally a huge step in that direction,” Sung said.
The research team, including Sung, tested a new treatment called AMT-130 on people who were in the early stages of HD. The treatment works by halting the part of the body’s gene production responsible for producing the toxic huntingtin protein. By targeting the messenger RNA that carries instructions from DNA to produce this protein, AMT-130 prevents its formation without altering the DNA itself—a key safety advantage over other genetic therapies.
The trial included 29 participants, some of whom received a low dose of AMT-130 and others a high dose, which is delivered to the brain during an eight- to 10-hour surgery. Of the 17 patients who received the high-dose treatment, seven are UAB patients.
After three years, those who received the higher dose showed a 75 percent slower disease progression compared to those who did not receive the treatment. The treatment helped trial participants maintain more of their movement, thinking, and daily functioning abilities without causing significant side effects.
 While invasive, this single-dose treatment is designed to last an entire lifetime, reducing the need for daily medication and having the possibility of a “one and done” treatment. Moreover, because the treatment does not permanently alter DNA, it avoids many of the risks associated with gene editing.
While invasive, this single-dose treatment is designed to last an entire lifetime, reducing the need for daily medication and having the possibility of a “one and done” treatment. Moreover, because the treatment does not permanently alter DNA, it avoids many of the risks associated with gene editing.
“We certainly remain cautious about interpretation of these results since they are only in a small number of patients, but the 75 percent disease-slowing is a big number and still very much a reason to be excited.”
The therapy has not yet been approved by the FDA; however, uniQure is seeking accelerated approval for the drug, which would be the first effective disease-modifying treatment option for HD patients.
“There is certainly still work to be done, as if this drug is approved, we as a community will have to figure out how to deliver this therapy to patients from a surgical and cost standpoint," Sung said. "But that is a problem I would welcome trying to solve as opposed to living in a world with no effective disease-modifying treatments for HD."
He continued: "I also think it is important to highlight the bravery of these 29 patients, a significant proportion of whom were our patients here at UAB, who underwent surgery to have a drug with permanent effects injected into the brain before we even knew if it was safe. But if their courage leads to the first FDA-approved disease-modifying therapy in HD, what a legacy that will be, and how exciting that UAB will have been such a big part of that.”
Additional details are available on ClinicalTrials.gov (NCT0543017, NCY04120493).