 On the second floor of Volker Hall, a group of first-year medical students gather in clinic practice rooms, their voices bright with energy as they run through patient histories and exam steps together. They compare notes, swap reminders, and encourage one another before stepping into a test session. These moments capture the essence of the Clinical Reasoning and Integrated Skills Program (CRISP), a pivotal element of the curriculum within the UAB Heersink School of Medicine. Launched in 2023, CRISP was built to ease the leap from the classroom to the clinic, giving students a structured, safe environment to build the skills—and confidence—they will need when they meet their first patients.
On the second floor of Volker Hall, a group of first-year medical students gather in clinic practice rooms, their voices bright with energy as they run through patient histories and exam steps together. They compare notes, swap reminders, and encourage one another before stepping into a test session. These moments capture the essence of the Clinical Reasoning and Integrated Skills Program (CRISP), a pivotal element of the curriculum within the UAB Heersink School of Medicine. Launched in 2023, CRISP was built to ease the leap from the classroom to the clinic, giving students a structured, safe environment to build the skills—and confidence—they will need when they meet their first patients.
For many students, that impact becomes clear once they begin clerkships. “CRISP allowed me to enter clerkships with a foundation of confidence that I believe I would not have had were it not a part of our curriculum,” said Rachel Frazier, MS3. Anna Townsend, MS3, echoed that experience: “It provided consistent practice of clinical skills with both real and simulated patients so that I could master skills and then practice them in a real situation… it made doing so on clinical rotations less intimidating.”
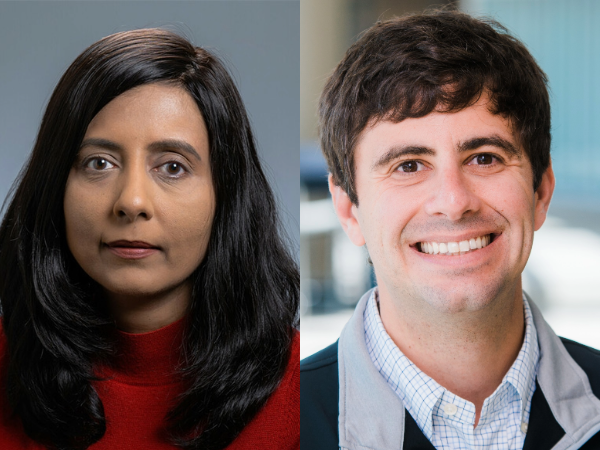
That sense of readiness reflects what Monica Agarwal, M.D., co-director of CRISP, has observed as the program has developed. In small groups led by faculty and supported by fourth-year students, medical students build confidence through repeated practice and feedback. By the time they reach clerkships, many are already comfortable with communication and patient care, allowing them to focus on more advanced skills. “Clinical reasoning is important—it’s in our name,” Agarwal said, “but it is also about communication and understanding how society and teams play a role, so that students are prepared to contribute and lead as collaborative members of their team, even as a third-year student.”
In July 2025, Zach Pacheco, M.D., joined Agarwal as co-director of CRISP. An emergency medicine physician and clerkship director, Pacheco brings a focus on preparing students to apply classroom learning directly to patient care. For him, CRISP’s greatest strength lies in how it pushes students to “think like physicians” earlier in their training. “It’s not just about being an information gatherer but about learning to synthesize that information into a patient plan,” Pacheco said. He also points to innovations such as point-of-care ultrasound, which allow students to bridge classroom science with bedside application in ways that will carry forward into their clinical years.
Alex Fresh, program director II for Undergraduate Medical Education, oversees the program’s daily operations and has watched students grow through its steady rhythm of “see one, do one, teach one.” “Students begin by observing a skill as it’s demonstrated, then practice it themselves, and finally reinforce their learning by teaching or offering feedback to their peers,” Fresh explained. She notes that the real turning point often comes when students recognize how what they’ve learned in lectures ties directly into CRISP sessions. That connection, she said, gives them a sense of pride and confidence as they prepare to work with real patients.
For Winter Williams, M.D., assistant dean for Clinical Education, the program’s impact is clearest in how it has become fully woven into the curriculum. “It was a separate course that existed outside other pre-clinical courses, and now it’s actually integrated into each course,” he explained. That shift allows students to connect classroom learning directly with patient cases in CRISP, reinforcing their understanding in real time. Looking ahead, Williams sees CRISP continuing to evolve, expanding across all four years of medical school and adapting to new tools such as artificial intelligence, while holding fast to its mission of preparing students to meet patients with skill, confidence, and compassion.
For students, CRISP is more than practice—it is preparation for the responsibility of caring for patients. For faculty, it is a chance to model the skills and empathy that define good physicians.