UAB Medicine is increasingly reaching beyond the confines of our healthcare facilities to provide world-class care for people where they are. Telehealth has become one of the most powerful tools in our mission to serve the people of Alabama, connecting patients across the state with UAB’s renowned experts, all without leaving their own communities.
UAB Medicine is increasingly reaching beyond the confines of our healthcare facilities to provide world-class care for people where they are. Telehealth has become one of the most powerful tools in our mission to serve the people of Alabama, connecting patients across the state with UAB’s renowned experts, all without leaving their own communities.
In June 2024, UAB eMedicine partnered with Whitfield Regional Hospital in Demopolis to launch the state’s first UAB Tele-Intensive Care Unit expanded hospital. For critically ill patients at Whitfield, this means round-the-clock access to UAB’s expert physicians and nurses. Less than a year later, in May 2025, the Tele-ICU celebrated its 500th admission—a testament to its lifesaving impact.
In September 2025, three more UAB Tele-ICUs went live at UAB St. Vincent’s Blount, St. Clair, and Chilton. These new sites reduce the need for patient transfers and in-person specialty consults, ensuring that high-quality critical care is available in more corners of the state.
Also in September, UAB eMedicine launched a pilot teletrauma program at Russell Medical Center in Alexander City and six UAB St. Vincent’s locations. The program seeks to enhance initial management of severely injured patients and expedite their transfer to a trauma center, and to identify patients who can be safely discharged home, thereby avoiding resource-intensive and costly trauma center transfers.
Digital innovation is only part of the story—UAB providers are also finding inventive ways to connect with patients in need on the ground. Alabama’s first street psychiatry clinic was established in late-2024 to provide care for Montgomery’s unhoused population. Led by Will Rutland, M.D., regional chair of Psychiatry at our Montgomery Regional Campus, and supported by trainees in the Montgomery Psychiatry Residency Program, the Homeless Outreach and Psychiatry Education, or HOPE Clinic provides care directly in the community, treating opioid use disorder, opioid overdose, and co-occurring serious mental illnesses.
Expanding psychiatric care in rural Alabama also took a major step forward with the launch of the Cahaba+UAB Rural Psychiatry Residency, which serves under-resourced sites in Bibb, Perry, and Wilcox counties and earned ACGME accreditation in 2025. Led by John Waits, M.D., the residency director and CEO of Cahaba Medical Care Foundation, the program welcomed its first three residents in June 2025. In all, UAB-affiliated psychiatry residency programs—including at our regional campus sites in Huntsville, Montgomery, and Tuscaloosa—are adding 18 mental health care residents to Alabama.

Equal Access Birmingham (EAB), Heersink’s medical student-run free clinic serving uninsured and underinsured people in our community, partnered with the Compassion Closet, another medical student-driven program, to provide clothing, shoes, hygiene items, and other essentials to people experiencing homelessness at EAB’s monthly Street Medicine Clinics.
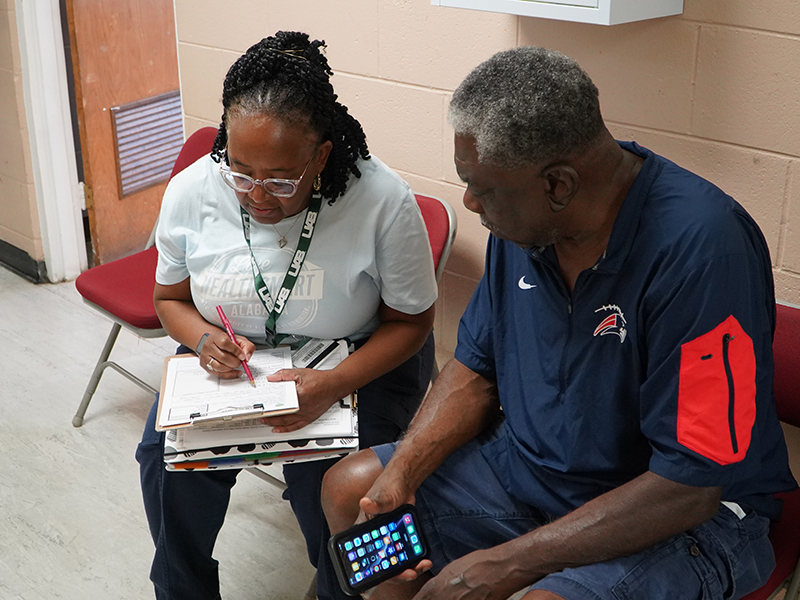
A grant from the Mike and Gillian Goodrich Foundation allowed Live HealthSmart Alabama, a UAB initiative to reduce the incidence of chronic disease across the state, to expand its Community Coach team in Selma and the Dallas County area. Community coaches are a crucial resource in areas where barriers to care are high and where rural hospitals struggle to meet the needs of those without primary care. The coaches guide residents through chronic disease management, refer them to appropriate healthcare resources, connect them to offerings for good nutrition and physical activity, and help them navigate challenges related to housing, food, transportation, and healthcare access.