Diverse Solutions to a Health-Care Shortage: Scholarship invests in the physician workforce of the future
Amiria Blakely and Jernell Simmons don’t need statistics to tell you the story of Alabama’s health care crisis. The two Heersink School of Medicine students grew up in communities without enough health professionals to provide care for the people living there. They have seen firsthand how a lack of access to medical expertise, particularly in rural and low-income areas, can impact health. And they are determined to do something about it by making a commitment to practice in underserved communities after graduation.
Today Blakely and Simmons are a step closer to their goal as the inaugural recipients of the new Karen McKoy, M.D., MPH, and Paul Lesser, M.D., Diversity in Medicine Endowed Scholarship. McKoy, a dermatologist and 1974 graduate of the School of Medicine, and Lesser, a gastroenterologist, made the gift to create the scholarship to help increase the diversity of the physician workforce, which is crucial for addressing Alabama’s health-care shortage, McKoy says. “It has been apparent for some time that many patients are most comfortable with someone with whom they can relate—who is close to their own racial and cultural identity,” she explains.
“The mission of the UAB Heersink School of Medicine is to train physicians to care for the people of Alabama, and in order to fulfill that mission, we must ensure that the next generation of physicians reflects the population of the state,” adds Craig Hoesley, M.D., senior associate dean for medical education. “Initiatives such as the Karen McKoy and Paul Lesser Diversity in Medicine Endowed Scholarship provide key support for attracting and retaining students who are historically underrepresented in medicine.”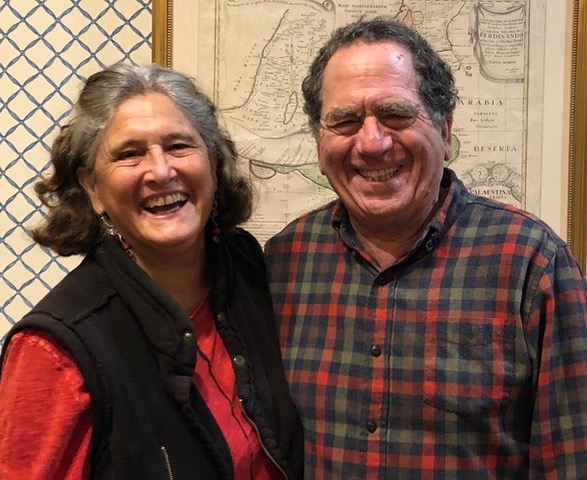 Karen McKoy and Paul Lesser
Karen McKoy and Paul Lesser
The Dean’s Office doubled the impact of the scholarship gift by matching McKoy and Lesser’s contribution dollar for dollar as part of its commitment to attract qualified students from populations that are underrepresented in medicine (URiM). That pleases McKoy, who treasures her ties to Alabama and received a merit scholarship from the state to attend medical school. “I feel indebted to Alabama for that start,” she says. Now she and her husband Paul, who split their time between Massachusetts and Georgia, want to “encourage graduates from UAB to stay and practice in their home state.”
That’s exactly what Blakely and Simmons intend to do. A Troy native and first-year medical student, Blakely aims to become a primary care physician to help “combat systemic disease that consistently impacts underserved communities,” she says. Simmons, a second-year student, says growing up in Selma, where finding a specialist was tough and many emergency cases were sent out of town, inspired him to pursue a medical career. When he graduates, he will be the first physician in his family, with plans to practice in a small city in need of health professionals.
The two students say the scholarship will ease the financial burdens and stresses of medical school, allowing them to concentrate on their studies—and their future goals. “I am truly honored to have the donors’ support,” Simmons says. “It feels good to know that I have amazing people supporting me and my dream.” – Charles Buchanan
The Dean's Office is matching gifts for URiM scholarships received through September 30, 2022, dollar for dollar up to $150,000. To learn more, contact Erica Hollins at 205-996-6839 or elhollins@uabmc.edu.
Compassion Inspires Compassion: Pulmonary gift benefits nurses and patients
Even in a hospital known nationally for excellence in patient care, some caregivers demonstrate a level of expertise and compassion that is unforgettable.
That has been the case for William Hutchins “Hutch” Cole Jr. and Jane Cole. When the couple sought treatment at UAB for Hutch Cole’s chronic pulmonary obstructive disease (COPD), they immediately were struck by the kindness of nurses Cindy Blackburn, R.N., and Jessica Nichols, R.N. “Both go beyond their duties to help him,” says Jane Cole. “Jessica has even gone so far as to give us her cell number when she is on vacation.”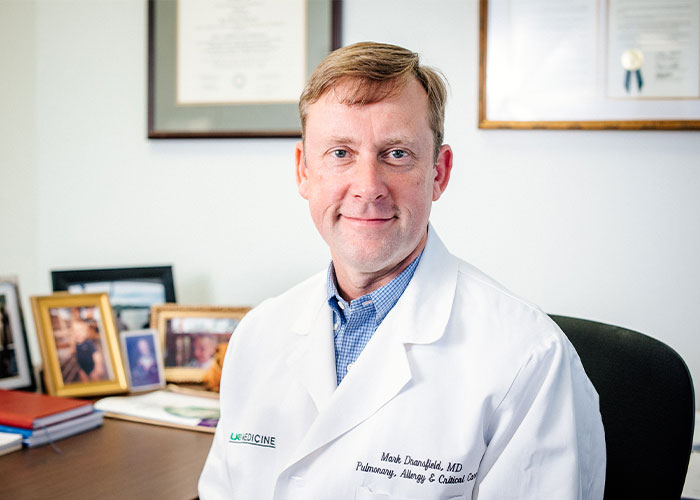 Mark Dransfield became director of the Division of Pulmonary, Allergy and Critical Care Medicine in August 2021.
Mark Dransfield became director of the Division of Pulmonary, Allergy and Critical Care Medicine in August 2021.
Grateful for the support and care they received from the nurses and from Mark Dransfield, M.D., Hutch Cole’s physician and director of the Division of Pulmonary, Allergy and Critical Care Medicine, the Coles are returning the favor by making a generous gift to the division.
Part of their gift will establish the Pulmonary Nursing Scholars Fund, which will reward the nursing staff for their dedication by supporting professional development. “This will lead to more learning opportunities, improved patient-care skills, and ultimately better patient outcomes,” says Dransfield, the William C. Bailey Endowed Chair in Pulmonary Disease.
The Coles are especially excited about the pulmonary Patient Assistance Fund, which will launch using the remainder of their gift. “Since we are financially blessed, my husband is able to access any medicine or equipment that he needs for COPD, but that is not true for all patients,” Jane Cole says. “Often insurance companies or Medicare will not pay for certain medications or equipment.”
Dransfield adds that his team often struggles to provide uninsured or underinsured patients with medical devices such as portable oxygen. “The Coles’ donation to establish the fund will allow us to provide those options to patients who otherwise could not have them.”
“We’re hopeful that others will contribute to this fund so that more patients can receive the best treatment available to ease their suffering,” Jane Cole says.
The Coles’ gift has already boosted the spirits of UAB’s pulmonary staff, who have had “a very difficult 18 months” caring for patients amid the COVID-19 pandemic, Dransfield says. “Our advanced practice providers, nurses, respiratory therapists, and physicians have been in near wartime conditions” that inflict a psychological toll. “Gifts such as the Coles’ help us to remember that the work we do every day makes a difference and is appreciated by our patients and their families.”
Dransfield is a nationally renowned expert in chronic obstructive pulmonary disease and has been the medical director of the UAB Lung Health Center since 2009. An elected member of the American Society for Clinical Investigation, he is the principal investigator for multiple clinical trials and observational studies sponsored by the National Institutes for Health, the United States Department of Defense, and the American Lung Association. – Charles Buchanan
To give to support pulmonary care and research at UAB, contact Christian Smith at (205) 934-1974 or christiannsmith@uabmc.edu.
A Lasting Tribute: Endowed professorship advances UAB’s brain cancer research efforts
After Austin Brown passed away from brain cancer in 2017 at the age of 35, his family wanted to do something special to honor those who cared for Austin, as well as those they came to know who dedicate their careers to finding a cure for the deadly disease that took his life. They especially wanted to honor Austin’s doctor throughout his five-year battle, Louis Burton (Burt) Nabors III, M.D. After meeting with representatives of the O’Neal Comprehensive Cancer Center at UAB, Austin’s parents, David and Janie Brown, and his wife, Mary-Margaret, decided the best way to accomplish this goal would be to establish an endowed professorship in Austin’s name.
In February 2021, Nabors, a professor and vice-chair for research in the Department of Neurology, became the inaugural holder of the William Austin Brown Endowed Professorship in the O’Neal Comprehensive Cancer Center at UAB. Austin Brown with his wife, Mary-Margaret, and their children
Austin Brown with his wife, Mary-Margaret, and their children
“We felt that the endowed professorship was a way to show our gratitude to Dr. Nabors for his care and commitment to Austin and others suffering from brain cancer, and to help ensure that those who follow in his footsteps at the Cancer Center have the resources needed to one day find a cure for brain cancer,” says David Brown.
Nabors says he has been moved by the Brown family’s commitment to advancing UAB’s brain cancer research, even after such a tragic loss. “They have maintained engagement and interest, which is a hard thing to do,” Nabors says. “Most of us when we’ve been through a hardship that’s tested us, we sometimes want to put that away and move on from it. But they maintained their support and worked hard to create this endowed professorship.
“The support we derive from the endowment allows us to keep moving our clinical research projects forward. It’s quite an honor for me to be the first person to hold this professorship.”
Austin was diagnosed in 2012 with glioblastoma, a high-grade form of the astrocytoma brain tumor for which there is currently no cure. Over the next five years he took part in several clinical trials in an effort to help discover any sort of breakthrough treatment.
“He had this incredibly unselfish attitude about the journey he was on. He was always such a willing participant,” David Brown says. “He was willing to try or do anything, not for himself but for his wife and children. Throughout it all his focus and concern were on his family.”
Nabors agrees. He says the entire Brown family was invested both in Austin’s personal treatment as well as the overall efforts in brain cancer research.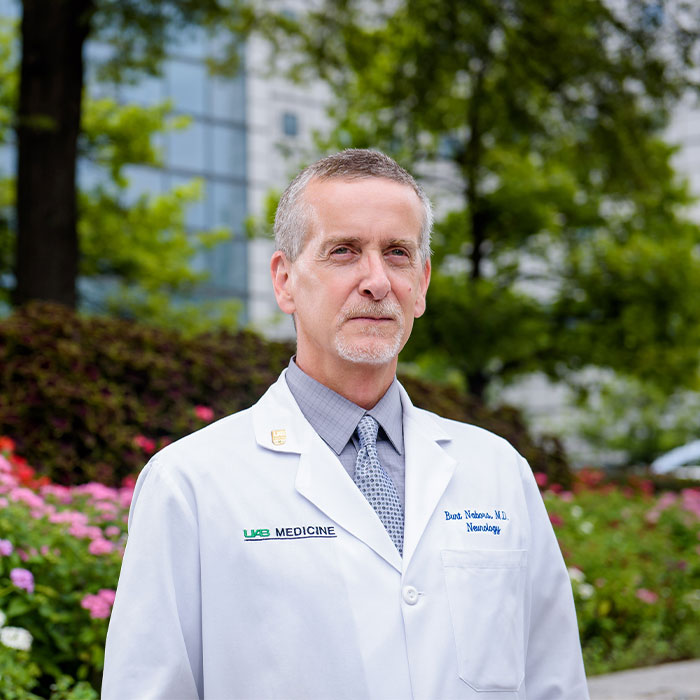 Burt Nabors is the inaugural holder of the William Austin Brown Endowed Professorship in the O’Neal Comprehensive Cancer Center at UAB.
Burt Nabors is the inaugural holder of the William Austin Brown Endowed Professorship in the O’Neal Comprehensive Cancer Center at UAB.
“Our meetings together were focused around Austin’s clinic visits. But usually within the context of that we’d discuss what was going on in research and what were some of the new opportunities,” Nabors says. “Austin participated in some of the Phase 1 studies at UAB. It takes a certain level of openness to be part of these when they’re in the early stages.”
While Austin was being treated, the Brown family established the Neuro-Oncology Acceleration Fund to support Nabors’ research efforts. Over the years, more than $1 million has been raised for the fund.
After Austin’s passing, the Brown family took up the cause of establishing the endowed professorship. As part of the fundraising, they hosted a dinner reception for approximately 20 people who had supported the Acceleration Fund or were supporters of the O’Neal Cancer Center. The goal was to raise $250,000 toward the endowed professorship. As it turned out, the hosts and guests contributed a total of $480,000.
“We invited friends, family members, and those we thought might have an interest in supporting the Cancer Center’s Neuro-Oncology Research Program, one of the finest in the country,” David Brown says. “We talked about the unique challenges associated with brain cancer research and invited the leadership of the Cancer Center along with Dr. Nabors to join us and explain to our guest how their funds would be used and the impact their support would have on his research.
“It’s always been my belief that donors will give more to a good cause if they know the people behind the cause they are being asked to support. That’s why we decided to host a smaller group in a more intimate setting and provide our guests the opportunity to meet and hear firsthand from the doctors they were being asked to support.”
Nabors currently maintains active basic, translational, and clinical research efforts. His laboratory is examining the role of RNA-binding proteins in neurological disease, particularly cancer, with an emphasis on therapeutic development. With the help of the endowed professorship, he says UAB will be able to expand such research programs.
“A lot of times when you have to go through the traditional pathways of NIH funding, it may take a long time,” Nabors says. “This gives us the ability to expand the projects we’re interested in, and also take on some things that might be a little riskier in terms of success.
“The brain is the most complex organ we have. It’s what defines us, all the things we feel, our emotions and behaviors. It’s an amazing organ, so we have to really work hard to better understand it and advance what we’re doing to improve patient outcomes.”
For the Brown family, that is the ultimate goal behind establishing the William Austin Brown Endowed Professorship. “We want to support Dr. Nabors and those who follow him,” David Brown says. “We want to provide those in our community who suffer with this disease the same care that Austin received and support the research at UAB that we hope will one day lead to a cure, all right here in Birmingham.” – Cary Estes
To learn more about supporting cancer care and research at UAB, contact Lisa Roth at (205) 934-0930 or leroth@uabmc.edu.
Selwyn Vickers, M.D., on his dual dean/CEO role
The turn of the New Year brought an exciting leadership transition to UAB, as UAB Heersink School of Medicine Dean Selwyn Vickers, M.D., FACS, assumed the role of CEO of the UAB Health System and CEO of the UAB/Ascension St. Vincent’s Alliance, while retaining his role as dean.
January 1, 2022, was the official date the transition took place, but the shift to a dual-role, CEO/dean leadership model had been carefully researched and planned. In fact, according to Vickers, it was the culmination of a shift toward greater alignment between the Heersink School of Medicine, the UAB Health System, and the University of Alabama Health Services Foundation (HSF) physicians’ practice plan begun under former School of Medicine dean and current UAB President Ray Watts, M.D. “When he was dean, Ray had the prior experience of being president of the HSF and interim CEO of the Health System. He had a conviction that the walls between those entities should come down, and he began the process of breaking down those barriers.” 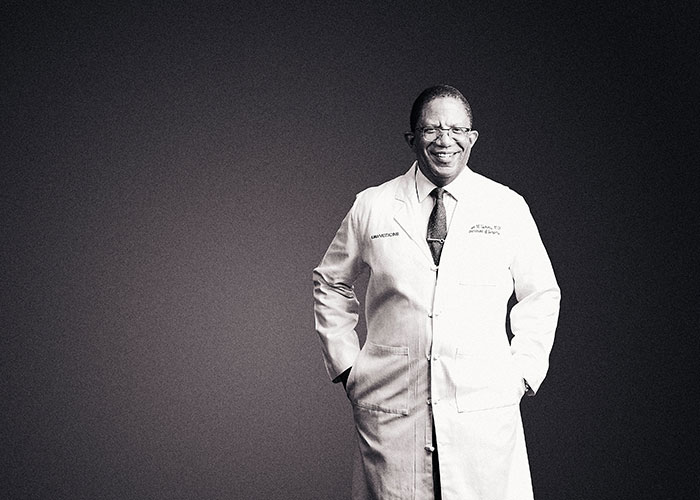 Vickers is the first person to be the medical school dean as well as the CEO of the UAB Health System and the CEO of the UAB/Ascension St. Vincent's Alliance.
Vickers is the first person to be the medical school dean as well as the CEO of the UAB Health System and the CEO of the UAB/Ascension St. Vincent's Alliance.
When former UAB Health System CEO Will Ferniany, Ph.D., decided he wanted to retire at the end of 2021 after nearly 13 years at the helm, he began meeting with Vickers, Watts, and other leaders to plot out the best way to ensure a smooth and effective transition. Through these talks, the plan to transform the leadership model to a single leader at the top began to take shape.
According to Vickers, the impetus for the change boils down to two words: alignment and excellence. “The structural change of our clinical enterprise’s leadership from two roles to one stems from the tremendous growth we have experienced over the past decade, thanks in large part to Dr. Ferniany’s strong leadership,” he says. “A key facet of my new role is identifying and fostering synergy between the lanes of academic research, patient care, and education and training. Ongoing alignment is achieved through our ability to create excellence in our individual lanes and uniting them for the shared goal of quality patient care.”
The CEO/dean leadership model is one that has been implemented successfully at a number of peer academic medical centers (AMCs) across the country, whose leaders Vickers consulted in planning for UAB’s transition. “The CEO/dean model is an operationalized strategy that has been successful for every AMC that has instituted it,” he says. “I met with leaders at Vanderbilt University, University of North Carolina School of Medicine, Johns Hopkins Medicine, and University of Michigan Medical School to hear and understand how their structures work.”
Those talks confirmed for Vickers and senior leaders that consolidating the roles of Health System CEO and Heersink School of Medicine dean to one person made sense for UAB. “A singular leader can fuse the interests of all groups at our enterprise and take a thoughtful approach to finances, operations, and outcomes of both worlds,” Vickers says. “My personal goal is to be a relational leader for every employee, faculty member, and trainee.”
A Leader’s Journey
Vickers’ unique combination of personal insight and earned expertise makes him ideally suited to tackle both the dean and CEO roles. At various points along his career path, he has been a medical student, resident and chief resident, practicing surgeon, researcher, and department chair, among others, giving him firsthand knowledge of the challenges confronting each group.
The many influences that guided him toward medicine start with his family. His parents, John and Clara Vickers, not only earned college degrees—a rarity for African-Americans living in Jim Crow-era Alabama—but they also both earned master’s degrees in education fields. His father went on to become one of the first 15 African-Americans to earn a doctoral degree from the University of Alabama. He later became dean of the School of Education at Alabama A&M University in Huntsville, where Vickers spent most of his formative years.
Vickers’ parents’ inherited their reverence for learning from their forebears. His paternal grandfather taught himself to read and write at age 44 and became mayor of his town. His maternal grandmother went to college for 10 summers to earn her bachelor’s degree and worked as a school principal in the 1940s. Her father studied under famed educator Booker T. Washington.
1986 M.D., John Hopkins University School of Medicine • 1986-1988 Surgical Internship, Johns Hopkins University • 1988-1990 Surgical Research Fellowship, Johns Hopkins University • 1990-1991 Registrar Surgery, John Radcliffe Hospital, Oxford, England • 1991-1993 Surgical Residency, Chief Residency, Johns Hopkins University • 1993-1994 Surgical Oncology Fellowship, Johns Hopkins University • 1993-1994 Instructor in Surgery, Assistant Chief of Service/Fellowship - Surgical Oncology, Johns Hopkins University • 1994-1999 Assistant Professor, UAB Department of Surgery • 1999-2003 Associate Professor, UAB Department of Surgery • 2000-2006 Chief, Section of GI Surgery, UAB Department of Surgery • 2001-2006 John H. Blue Chair of General Surgery, UAB Department of Surgery • 2002-2006 Co-Director, UAB Minority Health & Health Disparities Research Center • 2003-2006 Professor, UAB Department of Surgery • 2003-2006 Senior Scientist, O’Neal Comprehensive Cancer Center at UAB • 2006-2013 Jay Phillips Professor and Chair, University of Minnesota Department of Surgery • 2013-2021 Senior Vice President for Medicine and Dean, UAB Heersink School of Medicine • 2022 UAB Heersink School of Medicine, CEO, UAB Health System, and CEO, UAB/Ascension St. Vincent’s Alliance
The summer Vickers was 15, he visited his uncle, Leroy Vickers, M.D., in Cincinnati and shadowed him at his internal medicine practice for a week. “I still remember the elderly man with aortic stenosis he took me to see in the hospital,” Vickers says. “My uncle had seen him in his clinic and heard that very distinctive murmur. He got him into the hospital and got his valve replaced. The man was still recovering when we went by to see him, but he was so thankful because his quality of life was restored. I saw that man’s face when he saw my uncle, who was probably only 29 or 30 at the time, and I knew then that’s what I wanted to do.” Vickers performing surgery during his first tenure on the UAB surgical faculty, 1994-2006. Photo courtesy of UAB Archives.
Vickers performing surgery during his first tenure on the UAB surgical faculty, 1994-2006. Photo courtesy of UAB Archives.
Vickers attended Johns Hopkins for undergraduate, medical school, and postdoctoral training, during which time he honed in on his two abiding clinical and research passions: pancreatic cancer and health disparities.
He returned to Alabama in 1994 to join the UAB Department of Surgery as an assistant professor. He eventually rose to professor of surgery and became the first holder of the John H. Blue Chair of General Surgery, as well as the co-director of the UAB Minority Health and Health Disparities Research Center. In 2006, he was recruited to the University of Minnesota to become the Jay Phillips Professor and Chair of its Department of Surgery. In 2013, he was recruited back to UAB, this time to lead the School of Medicine as dean.
Vickers continues to perform pancreatic cancer surgeries, and his research has led to the development of important cancer treatments as well as crucial advances in the understanding of health disparities. He is a member of the prestigious National Academy of Medicine and is currently president of the American Surgical Association, the nation’s oldest and most prominent surgical organization. He continues to see patients and has had continuous National Institutes of Health (NIH) funding for more than 25 years. Even with these successes, he says the foundations of his life have always been “faith, family, and friends.”
All of these experiences, Vickers says, will inform his leadership style. “My personal growth goal is to be a relational leader for every employee, faculty member, and trainee,” he says.
The Dream Team
Famed longtime GE CEO Jack Welch said, “Before you are a leader, success is all about growing yourself. When you become a leader, success is all about growing others.” Vickers readily admits he will depend on a trusted, seasoned team of senior leaders to help him manage two highly demanding roles.
“I recognize that I cannot be everywhere all the time and I cannot be everything to everybody,” Vickers says. “Managing these roles will be largely driven by my reliance on the people serving in top leadership positions across the school and the UAB Health System. I want to position people so that the full scope of our academic mission can be front and center for all of our leadership.”
In the Heersink School of Medicine, Vickers says Executive Vice Dean Anupam Agarwal, M.D., will play a central role as “an important leader and figure for department chairs and faculty. Not only is he an accomplished scientist, but he is also accomplished in academic strategy. He has built great trust and confidence from people around him that will continue to serve us well.”
10 Questions with Dr. Vickers
Book you’re currently reading: The Speed of Trust by Stephen Covey
Favorite book: The Warmth of Other Suns by Isabel Wilkerson
Favorite local restaurant: Hot and Hot Fish Club
Favorite kind of pizza: Margherita
Favorite place you’ve visited: Cape Town, South Africa
Place you want to visit: Maldives
Favorite singer: Bill Withers
First concert: George Clinton and Parliament Funkadelic
Personal motto: Veritas vos liberabit (“The truth will set you free,” the Johns Hopkins University motto)
What makes you optimistic about the future?: I think we’ve overcome a lot more than we face now, both as a country and as a city, so I believe we have a very bright future ahead.
In the research realm, Senior Vice Dean for Research Etty (Tika) Benveniste, Ph.D., “will continue to lead with integrity and honor, as she has for several decades.” He especially credits her efforts around space and facilities, recruitment, and new research initiatives for helping grow the school’s research enterprise.
On the UAB Health System side, Dawn Bulgarella assumed a new position as president of the UAB Health System on January 1, in addition to the role of chief financial officer (CFO) that she has held since 2014. She is also the CFO for the UAB/Ascension St. Vincent’s Alliance and is responsible for combined annual budgets in excess of $5 billion.
“Our size and scope are major drivers to why we need both a president and a CEO in the Health System,” Bulgarella says. “As CEO, Dr. Vickers is going to be more outward-facing and involved in strategic direction setting, while I as president will maintain day-to-day responsibilities and partner with him and other senior leaders.”
Reid Jones became CEO of UAB Medicine in June 2020 after having served as chief operating officer of the UAB Health System since the position was created in 2013. “Reid has been a steady hand helping steer the Health System through many challenges and achievements during his long tenure,” Vickers says. “He has a deep understanding of the organization and his experience and expertise are key assets.”
Tony Jones, M.D., senior associate dean for Clinical Affairs in the Heersink School of Medicine, chief physician executive in the UAB Health System, and HSF president, is charged with maximizing practice efficiency and productivity, further improving quality and patient safety by promoting integration of the clinical service lines, and developing innovative, value-added care models. According to Vickers, “Tony is an accomplished academic physician executive who has extensive leadership expertise and the broad confidence and support of his physician peers.”
Vickers also says Jason Alexander, CEO of Ascension St. Vincent’s, will be a critical partner. “The St. Vincent’s Alliance has the potential to be transformative,” Vickers says. “We don’t have space to expand UAB’s footprint here in Birmingham. In order to continue growing the scope of our mission—from expanding access to care for our patients, to educating trainees, to growing our research—we need this alliance. So I am very excited by the synergies that exist between UAB and St. Vincent’s that benefit both our institutions.”
Vickers says he is particularly proud of the diversity of the senior leadership team. “I think we arguably have one of the most diverse teams in the country. It looks a more like the composition of our state, and it is a unique composition, I think, when you look across the country.”
The Path Forward
Alabamians have some of the most challenging health statistics anywhere in the United States: The state ranks 46th for obesity, 48th for diabetes, and 49th for high blood pressure. Among Vickers’ priorities as CEO is to continue building on and expanding the clinical excellence that he says Ferniany cultivated. “Because of Dr. Ferniany, the UAB Health System has transformed and grown,” Vickers says. “What excites me about the transition is the opportunity to create a truly national profile for our health system and our academic medical center. I want to see our institution gain the greatest level of national recognition for what it contributes, and to attract more exceptional people to come here.” Vickers says he is particularly proud of the diversity of the senior leadership team, and considers it one of the great strengths of UAB.
Vickers says he is particularly proud of the diversity of the senior leadership team, and considers it one of the great strengths of UAB.
In addition, Vickers says confronting socioeconomic barriers to health and health care is a key goal, and that strengthening UAB’s efforts to bring affordable health care to all people and regions of Alabama will be a hallmark of his leadership. “Alignment of key aspects of our mission will allow us to be our most effective and a potent force for affecting health care disparities, improving health outcomes, and relieving the burden of disease our patients face. The alignment we’ve been moving toward is really about a single focus: the health of our community. I want the clinical and research worlds to be oriented toward creating the best outcomes for our patients.”
As to what success looks like, Vickers says it’s about people. “I think success looks like we’re an organization that is concerned about every individual within it, from the environmental services staff to our busiest cardiac surgeon. I think it also looks like each part of our enterprise will continue to bring its best in education, research, and clinical care, and I see my job as bringing these teams closer together to work toward our ultimate mission of improving the health of all Alabamians and everyone who comes to us for care.” – By Jane Longshore and Mary Ashley Canevaro
A historic naming gift from an Alabama family will fuel the school’s next era of excellence
In September, the School of Medicine embarked on what promises to be an unprecedented era of growth thanks to a transformational $95 million lead gift from longtime University of Alabama at Birmingham (UAB) supporter Marnix E. Heersink, M.D., which was enhanced with a contribution of $5 million from Triton Health Systems. In recognition of this singular act of philanthropy, the school has been renamed the UAB Marnix E. Heersink School of Medicine. Along with a new name, the gift bestows a host of new opportunities and avenues of exploration, with implications for metamorphic change not just for the school but also for the city of Birmingham and the state of Alabama.
The gift’s impact will be felt across the school, accelerating and expanding our patient care, medical training, and research and innovation enterprises, especially in focus areas such as precision medicine and pharmacogenomics, cancer biology, neurosciences, health disparities, and immunology, among others. The largest portion of the gift will be used to support priority initiatives and recruitment and retention of faculty leaders in the Heersink School of Medicine. The remainder of the gift has established two new institutes in areas of passionate interest for both the school and the Heersink family: the Marnix E. Heersink Institute for Biomedical Innovation and the Mary Heersink Institute for Global Health. The gift will also establish the Marnix E. Heersink Institute for Biomedical Innovation Endowed Support Fund and name the Heersink Biomedical Innovation Conference Center. Marnix E. Heersink, M.D., and Mary Heersink, longtime supporters of UAB and the School of Medicine, have made a $95 million gift to name the UAB Marnix E. Heersink School of Medicine, as well as establish two new institutes.
Marnix E. Heersink, M.D., and Mary Heersink, longtime supporters of UAB and the School of Medicine, have made a $95 million gift to name the UAB Marnix E. Heersink School of Medicine, as well as establish two new institutes.
“This historic gift reflects both Dr. Heersink’s heart for service and the scale of our shared ambition for the School of Medicine to be a global leader in biomedical discovery and innovation, medical training, and patient care,” says Selwyn Vickers, M.D., FACS, dean of the UAB Heersink School of Medicine and CEO of the UAB Health System and CEO of the UAB/Ascension St. Vincent’s Alliance. “It is a powerful affirmation of the unlimited potential of our school and reinforces what we have always known: that UAB truly is a world-class institution.”
The Road to Naming
It’s an elite league with names familiar to people inside and outside the medical field: Pritzker, Weill, Perelman, Feinberg, Geffen—all philanthropist-named medical schools, among them some of the most prestigious in the U.S. The Heersink gift is not only the largest in the university’s history, it is among the top 200 private gifts made to higher education since 2017, according to The Chronicle of Higher Education.
The gift came about through a combination of intention and synchronicity. Several years ago, the Dean’s Leadership Team created a strategic plan outlining the school’s ideal growth and the tactics to achieve such growth, including naming the school. “In a short amount of time, just three years, we were able to reach our goal,” says Anupam Agarwal, M.D., executive vice dean in the Heersink School of Medicine. “It was part of our strategy for growth.”
From the beginning, it was important to school leaders to build ethics and values into the strategy of securing a philanthropic gift to name the school. Finding the right donor was key. “Dr. Vickers wanted to seek out a donor aligned with our school’s vision and goals—someone who knew the unique issues of health care, health equity, and barriers in the state of Alabama,” Agarwal explains.
They found that sought-after alignment in Marnix Heersink, M.D., his wife Mary, and their family. The Heersinks are well-known philanthropists in Alabama and beyond, having made significant gifts from their personal funds and through their family foundation. Previous gifts and pledges to UAB include those to renovate the atrium and establish the Heersink Family Active Learning Resource Center in the School of Medicine’s Volker Hall, the Heersink Family Endowed Glaucoma Fellowship, and the Heersink Family Foundation Scholarship Endowment in Optometry, among others.
For their part, the Heersinks made a strategic decision to invest in a medical school with a record of excellence and an upward trajectory of success, criteria the School of Medicine more than meets. The school has experienced remarkable growth under Vickers’ leadership, notably in research funding. In 2018, UAB became part of an elite group of eight academic medical centers that had attained more than $100 million in net NIH funding growth over the previous five years and was the only school to rise 10 spots in five years. According to preliminary data, in 2021 the school ranked No. 21 in NIH research funding with $272 million, placing us on the cusp of achieving our goal of a top 20 NIH ranking.
Marnix Heersink says his confidence in the school’s leadership partly inspired the gift. “The leadership at UAB is respected across the nation,” says Marnix Heersink. “People are aware of Dr. Vickers and the team that he’s recruited. I see this gift as an opportunity to endorse that leadership and watch what happens. It’s an investment that I know will be put to good use.
“I use the acronym GIVE: Gratitude is the first letter—our family was educated here and received health care here, and we’re very grateful for that. The I is for investment—I do believe this gift is an investment in a school that is rising and is only going to get better. And then there’s Values and Vision—the school’s values and vision align perfectly with our family, and I truly believe in what the school stands for. And the last word is Excellence—I believe the things that are being done here exemplify excellence, and I think the whole state should be proud of that. So those four letters are the reason the gift was given.” The Heersinks arrived in Dothan, Alabama, in 1978 with, as Dr. Heersink says, “a used car, some clothes, and a lot of love and hope. And great educations.”
The Heersinks arrived in Dothan, Alabama, in 1978 with, as Dr. Heersink says, “a used car, some clothes, and a lot of love and hope. And great educations.”
A Family Dedicated to Service
The denizens of Dothan, Alabama, are long familiar with the Heersink family. “Mary and I came to Dothan in 1978,” says Marnix Heersink, a renowned eye surgeon, innovator, and entrepreneur. “We had in our possession a used car, some clothes, and a lot of love and hope. And great educations.”
The Heersinks’ journey to Alabama started in Europe. Marnix Heersink was born in The Netherlands, where his father was a civil servant who served as mayor of the family’s hometown. The family immigrated to Canada, where his father’s counsel helped guide Marnix toward a career in medicine. “My dad was a very wise man, and when I was about 16 he sat me down and said, ‘What do you want to become?,” Marnix recalls. “I didn’t really know, so he said, ‘Okay, tell me what you don’t want to be.’ We talked and he said, ‘It sounds like you want to be able to do things for other people.’ We checked down a list of possibilities and I realized I needed to keep medicine in the forefront of my mind. That was probably the start of me thinking about a career in health care.”
Marnix Heersink earned a medical degree from the University of Western Ontario in Canada. He completed an internship at the Royal Victoria Hospital in Montreal and an ophthalmology residency at Wills Eye Hospital in Philadelphia, followed by a fellowship in cataract surgery and intraocular lens implantation.
It was during his training in Philadelphia that Marnix met and married Mary Parks, the daughter of renowned pediatric ophthalmologist Marshall Parks, M.D., considered the “father of pediatric ophthalmology.” Parks inspired a reverence for medicine in his children. “In my household growing up, I saw that there was very little division between our family life and his profession,” Mary Heersink says. “His office was attached to our house, so on a typical Sunday afternoon there would be a child knocking on the door because he had an eye injury. Patients were in and out of our home, and teachers and fellows from all over the world visited us. So I grew up with the idea of medicine being an all-encompassing, sacred trust.”
When Marnix completed his training, he and Mary set off to find a location to establish his practice. Dothan was one of several places they visited and they say they immediately felt welcome in the community. In fact, on their first visit to the city, the couple bid on a house they say they knew would be their future home before ever setting foot inside.
Within two years of their arrival in Dothan, Marnix Heersink co-founded Eye Center South with John Fortin, M.D., which in the decades since has grown to 12 locations across Alabama, Georgia, and Florida. In 2019, Marnix Heersink and his family opened Health Center South, a 140,000-square-foot, state-of-the-art medical complex for doctors of all specialties in Dothan. He is also an owner or agent of many other companies, including real estate holdings and manufacturing entities in the United States and abroad.
Since 2017, Mary Heersink has been an invaluable source of counsel as a member of the School of Medicine’s Board of Visitors. She is an internationally known food safety advocate and the author of “E. Coli O157: The True Story of a Mother’s Battle with a Killer Microbe.” In it, she recounts the harrowing experience of her then 11-year-old son Damion, who nearly died from E. coli in the early 1990s. She was inspired to co-found STOP Foodborne Illness, a national grassroots organization dedicated to preventing illness and death from foodborne pathogens. STOP is widely credited as being the driving force behind the passage of the Food Safety Modernization Act of 2011. She is a member of the Advisory Board of the Master of Global Health Program, a joint initiative among McMaster University in Canada, Maastricht University in the Netherlands, Manipal University in India, and Thomassat University in Thailand. She has also served on boards of directors for numerous nonprofit and civic organizations in the Dothan area, including Girls Clubs of Dothan, the Wiregrass Museum of Art, and Landmark Park.
The Heersinks’ commitment to service is perhaps best expressed through their six children, all of whom have pursued careers in health care: ophthalmologists Mila, a Heersink School of Medicine graduate, and Sebastian, an MIT and Georgetown Medical School graduate; Bayne, a dentist who graduated from the UAB School of Dentistry, including a two-year UAB prosthodontic fellowship; Damion, a licensed U.S. patent attorney who earned a Master of Public Health degree from UAB in 2005 and has since earned his medical degree and is now training to become an internal medicine physician at Ochsner Health in New Orleans; and twins Christiaan and Marius, who followed the example set by Mila by participating in UAB’s Early Medical School Acceptance Program and who earned combined M.D./MBA degrees from UAB and are currently in ophthalmology and family medicine residencies, respectively. The Heersinks’ daughter-in-law Juanita Titrud Heersink, M.D., was Ms. UAB in 2003, graduated from the School of Medicine, and completed her internal medicine residency at UAB. The Heersinks' gift established two new institutes in the school: the Marnix E. Heersink Institute for Biomedical Innovation and the Mary Heersink Institute for Global Health.
The Heersinks' gift established two new institutes in the school: the Marnix E. Heersink Institute for Biomedical Innovation and the Mary Heersink Institute for Global Health.
An Era of New Promise
What is the gift’s significance for the school’s research, patient care, and medical education missions, and how will it impact the school’s future? A large portion of the gift will be used to establish endowments, which are critical for fostering excellence across all our mission areas. That’s because endowments aren’t just about prestige—they are about people, enabling the School of Medicine to recruit and retain the most talented faculty and expanding the possibilities of what we can achieve.
“A combination of new endowed chairs and endowed professorships offers a tremendous opportunity for us in terms of recruitment of new faculty as well as retention of some of our outstanding faculty,” says Tika Benveniste, Ph.D., senior vice dean for Research. “The gift helps us be more competitive with our peer institutions because we can offer protected time for specific research. In addition, these endowments will live at a school-level, so no matter which department a faculty member is appointed to they can be nominated.”
In the clinical care realm, endowed positions increase our capacity to provide innovative patient care, so people don’t feel the need to travel outside the state for specialized treatment. And of course, talented faculty enrich the learning experience immeasurably for medical students and residents, becoming trusted and influential mentors and helping mold trainees into tomorrow’s leading physicians and scientists.
As Agarwal points out, the core of all these enterprises is the same: the patient. “Why are we doing research? To impact and improve patient care. Why do we focus on clinical practice? To treat patients better. Why do we train and educate? To build on research, while training the future generation to treat patients. This gift will benefit all three areas.”
Likewise, the two newly established institutes will increase our capacity and strengthen our efforts in two key focus areas, with benefits that will echo across all mission areas. Led by Alan Tita, M.D., Ph.D., associate dean for Global and Women’s Health in the Heersink School of Medicine, the Mary Heersink Institute for Global Health seeks to improve overall health and well-being and promote equity in health outcomes among people around the world. The institute is building a coordinated, comprehensive, and sustainable infrastructure for the Heersink School of Medicine, UAB, and international partners to help foster educational opportunities, facilitate high-quality biomedical research, and provide services and capacity-building support—all geared toward addressing the most pressing and complex global health challenges.
Tita says the COVID-19 pandemic illustrates perfectly why the time is ripe for the institute. “The pandemic has shown us how interconnected the world really is, and that what happens elsewhere in the world impacts our health here at home. The world is becoming smaller—with faster travel and digital technology and new innovations, we interact and connect with the rest of the world on day-by-day, minute-by-minute basis, so being engaged in global health is in our interest.”
Despite that interconnectivity, disparities in health and health care access—both within the U.S. and across the globe—are glaring. Tita says having robust global health programs will better equip UAB to improve the health of vulnerable populations here at home as well as internationally. “For example, cardiovascular disease is a major cause of death here in Alabama, and is also a major cause of death in many other, less developed countries,” he says. “If we can coordinate across these countries and act together, we bring more to the table to overcome our common challenges.”
Similarly, the Marnix E. Heersink Institute for Biomedical Innovation, led by Rubin Pillay, M.D., Ph.D., assistant dean for Global Health Innovation in the Heersink School of Medicine and chief innovation officer of the UAB Health System, is establishing a framework for what Pillay calls “sustainable innovation” in health care delivery. Innovation involves the spark of creativity and ingenuity, he says, but to make it sustainable you need intention, infrastructure, and support, and that’s where the institute comes in.
“The health care sector in the United States is plagued with sky-high costs, unequal access, and erratic quality,” Pillay says. “The purpose of the institute is to put together a team that is focused on transforming and innovating health care delivery and addressing the quadruple burden of health care cost, quality, access, and experience.”
An important element of the institute will be The Clinic at UAB. “This is the equivalent of an innovation center, where a lot of the applied activities are going to take place,” says Pillay. “Physicians, nurses, staff who have ideas and solutions they’d like to explore can come to the Clinic, and we will help navigate the process and provide the necessary support. And within the clinic we’ll have boot camps and training initiatives.” A satellite location, The Clinic at Dothan, will extend the institute’s mission to rural Alabama.
Education and training will also be a major objective of the institute. “Innovation requires a skill set. We are going to launch a master’s degree in health care innovation, which we believe will be the first master’s in health care innovation delivered by a medical school globally. We will also launch a series of graduate certificates, in AI (artificial intelligence) in medicine, digital health care, and health care innovation.”
Innovation even impacts how the institute plans to deliver its programs and services. “We want to be essentially the first academic program delivered in the metaverse,” Pillay says. “We are going to use a combination of mixed and augmented reality, which will give students, whether they are in Dothan or Mumbai, the same immersive experience that our students in Birmingham get.” In addition to naming the school and creating two new institutes, the Heersink gift also named the Marnix E. Heersink Institute for Biomedical Innovation Conference Center.
In addition to naming the school and creating two new institutes, the Heersink gift also named the Marnix E. Heersink Institute for Biomedical Innovation Conference Center.
The Road Ahead
While the school’s name may have changed, the qualities that make it worthy of this powerful philanthropic endorsement remain the same: the focus on collaboration and innovation; the ability to respond to the needs of the community; the audacity to dream big dreams and do big things; and above all, the focus on delivering world-class, patient-centered care.
School leaders say the gift will have a domino effect on our surrounding community and the state at large. While the gift will directly strengthen and augment the school’s strategic goals across our mission areas, “it is also going to be a driver for the economic engine of UAB—and by extension Birmingham and the entire state of Alabama,” says Benveniste.
That is just what Marnix Heersink hopes the gift will achieve. “We hope the spinoff from the gift will be of benefit to people who aren’t even at the university—people across the city and state,” he says. “I hope the whole state will be lifted up by what happens here.” – By Jane Longshore and Mary Ashley Canevaro
Immunology Institute fosters collaboration to harness the power of the immune system to fight disease
When the COVID-19 pandemic erupted in early 2020, immunologists leapt into action. Here was a disease that looked familiar in many ways—a respiratory coronavirus like SARS and MERS, which they had studied for years. But they also were primed to investigate COVID’s more curious impacts on other parts of the body, as well as the lingering symptoms known as “long COVID,” because immunologists are literally everywhere in medicine.
They’re part of the teams studying infectious diseases, of course, but you’ll also find them alongside pulmonologists, cardiologists, gastroenterologists, oncologists, rheumatologists, neurologists, and many others. If the specialty concerns an organ or disease touched by the immune system—which is pretty much all of them—then an immunologist is involved.
UAB’s new Immunology Institute aims to connect all that expertise, linking more than 100 immunologists across the campus to answer a common question: How do you identify the treatment that works best for each patient, whether for COVID, cancer, or another disease? “We want to find biomarkers we can use to predict outcomes and select therapies that may be the most effective,” says Frances Lund, Ph.D., former Charles H. McCauley Chair of Microbiology, who serves as the institute’s founding director. The leadership team also includes associate directors Troy Randall, Ph.D., the Meyer Foundation William J. Koopman, M.D., Endowed Chair in Immunology and Rheumatology, and Paul Goepfert, M.D., the Edward W. Hook III, M.D., Endowed Professor in Infectious Diseases.  Fran Lund is the inaugural director of the UAB Immunology Institute
Fran Lund is the inaugural director of the UAB Immunology Institute
The institute, one of only a few nationwide, will provide the infrastructure to foster translational research, which will strengthen partnerships and an exchange of knowledge between basic and clinical scientists. For example, Lund explains that those clinical scientists will be able to use immunological assays in their trials so that they “understand not only how a therapy affects the end stage of a disease, but also how it works within the patient.” At the same time, basic scientists will be able to move their studies beyond animal models to people. “That jump is hard,” Lund says. “We can make those experiments possible by connecting them with clinical researchers who have access to samples and understand human disease.”
Lund highlights some current interdisciplinary research that represents the kinds of breakthroughs you can expect from the Immunology Institute:
Targeting Difficult Tumors
Lund is fascinated by the fact that scientists can teach the immune system to recognize and eliminate threats. Vaccines are one way to do that. Immunotherapies, which target cancer, are another—and pioneering UAB research is making them effective against tough-to-kill tumors.
In a first-of-its-kind phase 1 trial, Pediatrics professor Gregory Friedman, M.D., treated malignant pediatric gliomas in the brain with HSV-1 G207, a modified form of the herpes virus that causes cold sores. Once injected into the tumor, G207 replicates and kills cancer cells while triggering a strong immune response to the glioma. Eleven of the trial’s 12 patients responded to the treatment, with an overall survival rate that was more than double the median survival rate—less than six months—for children with progressive or recurrent high-grade gliomas. Some patients lived longer than 18 months.
“After treatment we saw a dramatic increase from few immune cells, or a ‘cold’ tumor environment, to numerous immune cells, or ‘hot,’ environment,” says Friedman, who also is a scientist in the O’Neal Comprehensive Cancer Center at UAB. “This is a critical step in the development of a safe, effective immunotherapy” for these pediatric gliomas, with less toxicity than chemotherapy and radiation.
A planned multi-institutional phase 2 trial could shed light on the optimal timing for treatment, as well as therapies that can be combined with G207 to magnify the anti-tumor immune response. Friedman’s team also is continuing another phase 1 trial to treat recurrent pediatric tumors like medulloblastoma that may have greater sensitivity to G207.
Meanwhile, Masakazu Kamata, Ph.D., an associate professor of Microbiology, is solving a different problem. Laboratory-produced monoclonal antibodies like rituximab have revolutionized cancer treatment by sticking to proteins on cancer cells, thus triggering the immune system to attack and kill the cells. But they don’t work well against tumors in the adult central nervous system (CNS) and lymph nodes simply because they are too large to move through the barriers protecting those organs. So Kamata and his team have shrouded rituximab in a thin polymer shell that includes connection points for cellular receptors, allowing it to slip past the blood-brain barrier and hitch a ride on immune cells to enter the lymph nodes. Studies in animal models revealed that a single cycle treatment increased rituximab levels in both areas, leading to “complete remission of all lymphomas including CNS-metastasized lymphomas,” Kamata says. Now the nanocapsules could open doors for monoclonal antibodies to treat other neuro-brain diseases, he adds. Left to right: Immunology Institute Director Fran Lund with associate directors Paul Goepfert and Troy Randall.
Left to right: Immunology Institute Director Fran Lund with associate directors Paul Goepfert and Troy Randall.
Protecting Preemies from Infection
The front lines of the body’s defenses run through the gut. That’s where most of the immune system comes face to face—or cell to cell—with an abundance of external pathogens. Yet in extremely premature infants, whose intestines are still developing after birth, invading bacteria can get the upper hand. Overgrowth of a species such as Klebsiella pneumoniae can spread into the babies’ bodies, raising the risk of life-threatening infections known as late-onset sepsis (LOS).
A UAB research team including Casey Weaver, M.D., and Michael Gray, Ph.D., found that these problematic bacteria share a common trait: “Unlike the bacteria that dominate a healthy microbiome, those that can cause LOS are able to use oxygen,” says Gray, an assistant professor of Microbiology. “Our results suggest that the amount of oxygen in the infant gut is an important factor in the development of LOS.”
Even more exciting, the investigators discovered that the presence of Lactobacillus murinus bacteria in the intestines seems to have a protective effect. In animal models, L. murinus dramatically reduced K. pneumoniae overgrowth when it was given before the LOS-triggering pathogen was introduced. Weaver, the Wyatt and Susan Haskell Endowed Professor for Medical Excellence in Pathology, says the result shows that “normal constituents of the microbiome in the neonatal gut are both necessary and sufficient” to help prevent LOS.
The discoveries could have implications for maternal and neonatal antibiotic use, which can impact protective bacteria in the infant microbiome. In addition, the National Institutes of Health recently awarded the team a grant to research the molecular mechanisms that enable those bacteria to prevent LOS. Identifying those could lead to the development of probiotics for human preemies. “The microbiome and its interactions with the immune system are complicated,” Gray says. “There’s a lot of work to do to figure out the detailed connections and causal relationships that would allow us to understand when probiotics would be the most effective treatments for specific diseases.”
Collecting Clues to Decipher COVID
In February 2020, Nathan Erdmann, M.D., Ph.D., marshaled a team to begin collecting COVID-19 samples from patients—even before the pandemic hit Alabama. “We recognized there was going to be a fair degree of chaos,” says Erdmann, assistant professor in the Division of Infectious Diseases. And in that situation, “one of the most valuable things for investigators is high-quality samples, particularly from patients with severe disease.” That preparation paid off: Not only was UAB ready to collect samples from its first COVID patient, but the team also could compare them with patient samples of typical seasonal coronavirus, providing an early understanding of immunological responses to the novel virus.
Today the Enterprise COVID biorepository includes blood, urine, saliva, and swabs from a cohort of nearly 4,000 patients, including 3,300 acute patients. Samples also represent deceased patients, vaccinated patients, and a control group. Altogether, the collection outlines a history of the pandemic in the region, which makes it unique, Erdmann says. “As things evolve, we’re able to reference the various phases of the illness and its strains as well as the native immune response to different treatment strategies.”
Collecting multiple samples from, in some cases, very sick patients in a hospital on lockdown was a challenge that no one person or lab could have accomplished, Erdmann says. Because hospital access was limited, he worked with clinical staff and UAB’s Institutional Review Board to obtain verbal consent from patients—and often found himself answering nurses’ questions at 2 a.m. The UAB Center for Clinical and Translational Science (CCTS) expanded the biorepository’s umbrella to include samples collected and processed by the Microbiology and Pathology departments.
More than 50 research teams representing myriad disciplines have worked with the biorepository to discover crucial details about COVID, says Jennifer Croker, Ph.D., CCTS senior administrative director and assistant professor of Medicine. Samples have helped investigators shed light on viral variants, testing methodologies, infection outcomes in immunosuppressed patients, and potential triggers for “long COVID,” for example. Others have demonstrated the role of early antibody responses in helping to prevent serious infection—and revealed that many infected patients don’t develop antibodies, emphasizing the importance of vaccination. Future research could provide clues to predict COVID severity and pave the way for new vaccines. – Charles Buchanan
Called to Care: Meet students who are determined to bridge gaps in rural medicine
When they look toward their future in medicine, UAB Heersink School of Medicine students Carla Brown and Ellie Pitchford both envision practicing medicine in rural communities similar to the ones that shaped them.
Growing up in Batesville, Mississippi, Brown, who will complete her third and fourth years at the school’s Tuscaloosa Regional Medical Campus, saw how people in the small, rural town cared for each other, but also how they struggled to access high quality, timely medical care, particularly if they needed to see specialists or were facing an emergency. Left to right: Carla Brown and Ellie Pitchford
Left to right: Carla Brown and Ellie Pitchford
“We have one or two family medicine physicians who I have known my whole life, and a small hospital that has threatened to close several times. We do not have a lot of specialties; they just got rid of labor and delivery,” Brown says. “Growing up in that environment, I have seen several people in life-or-death situations need to get to the nearest hospital with specialists who can treat them and unfortunately pass before they can make it there.”
Raised roughly 200 miles from Birmingham in Scottsboro, Alabama, Ellie Pitchford noticed similar trends as friends and family sought medical care. “My grandparents often had to travel 45 minutes to see their primary care provider,” says Pitchford, who lived in Scottsboro until age 21, when her family moved to Birmingham. “There is also a significant lack of mental health resources in rural communities, something that I would like to address as a provider and make available to my patients.”
A lack of access to primary care is a growing problem in Alabama’s rural areas. “Currently, our state needs more than 600 additional primary care providers to meet the needs of the patients and the kinds of health conditions that we will be seeing by 2030,” says Irfan Asif, M.D., chair of the Department of Family and Community Medicine and associate dean for Primary Care and Rural Health. “To address this deficit, we must be aggressive in the family medicine and primary care programming that we develop and implement.”
Both Brown and Pitchford are first-year students and members of the latest cohort of the UAB Department of Family and Community Medicine’s Comprehensive Urban Underserved and Rural Experience program, or CU2RE. Launched in 2020 through a $7 million grant from the Health Resources and Services Administration, CU2RE is designed to enhance the recruitment, training and retention of medical students dedicated to serving as family medicine physicians in underserved rural and urban areas of Alabama. In 2021, CU2RE was awarded $5.2 million in supplemental funding from HRSA to expand and continue its mission and support programming around the state.
The program admitted a second cohort of 16 students in fall 2021, including Brown and Pitchford, after launching with an inaugural cohort of eight students in 2020. Students, who can choose between an urban underserved and rural medicine track, remain in the program throughout their four years in medical school. They are paired with a dedicated mentor and complete web-based modules, have monthly early clinical experiences with a family medicine preceptor, and work through an intensive summer program during their first two years, along with a four-week Family Medicine Clerkship in their third year and a four-week Family Medicine Acting Internship in their fourth year. A hallmark of the program is a 10 patient panel that each student will care for to improve the quality of their health through methods such as health coaching. CU2RE participants took part in a dermatology workshop in summer 2021.
CU2RE participants took part in a dermatology workshop in summer 2021.
“I am excited about getting a lot more hands-on experience early in medical school and about the mentorship aspect of the program,” Brown says. “I did not really have a lot of guidance getting to medical school, so it was very important to me to find that here. I am also excited to be with others who are interested in primary care and family medicine, to bounce ideas off each other and share experiences that might be different from those I have had.”
Pitchford, who will complete her clinical years at the Huntsville Regional Medical Campus, says she applied to CU2RE because she is “hungry for clinical opportunities to start serving people now, instead of having to wait.”
“Growing up, I always saw the doctors [in Scottsboro] use medicine as a way to serve people and that is what attracted me to medicine,” she says. “If I am going to spend all of this time in school, I want to come out of it able to serve people and serve some of the most vulnerable populations, including rural people.”
Both women believe that an influx of family medicine and primary care physicians, supported by programs like CU2RE, can help solve some of the problems patients face in rural areas. “I saw a lot of health disparities in my community, which really made me want to practice in a similar area,” Brown says. There are a lot of different challenges, she said, from gaps in communication that keep patients and providers from understanding the patients’ concerns and how to treat them, to logistical challenges like transportation to and from appointments.
Pitchford also wants to make one thing clear to her classmates and fellow aspiring physicians: providing care in rural communities is challenging, meaningful, and valuable work. “I think sometimes there is this expectation or bias that medical students who are interested in rural medicine are limiting themselves or taking the easy route,” she says. “I want people to be encouraged. You are not limiting yourself in rural medicine. Medicine is all about serving the patient and you will do that every day.” – By Caroline Newman
Step by Step: Medical student helps rebuild lives of those impacted by homelessness through running
At the Heersink School of Medicine, it’s commonplace for students, staff, trainees, and faculty alike to blend their professional interests with service work. During the height of the coronavirus pandemic, health disparities were more illuminated nationally than ever before, and opportunities for community outreach abounded.
One group of interdisciplinary students recognized a need among one of Birmingham’s most marginalized populations—those affected by homelessness. In the fall of 2020, James Harris, MS3, was compelled by the uncertainties of the pandemic to find ways to help homeless populations in Birmingham. Left to right: Jordan George (MS3), James Pate (MS4), George Campbell (R2R client), and James Harris (MS3).
Left to right: Jordan George (MS3), James Pate (MS4), George Campbell (R2R client), and James Harris (MS3).
To support the emotional, mental, and physical needs of the homeless population in Birmingham, Harris—along with a few of his Auburn University alumni peers Jordan Carr, Garrett Rogers, and Jesse Westerhouse—started Run 2 Rebuild, an organization that provides a support network, motivation, and physical fitness education to the men of Birmingham’s Jimmie Hale Mission (JHM).
Harris says each of the founding members has a passion for running. “We have seen the beneficial traits that develop from this activity and the way it positively affects all areas of our lives. We wanted to find a way to share this passion and make an impact on individuals facing addiction or homelessness in Birmingham,” Harris says.
“Our ultimate goal is to use running, goal setting, and camaraderie to help others reach their full potential in all areas of life. We began conversations with Michael Coleman, the director of Jimmie Hale Mission, in September 2019, and we officially launched a Pilot Program in early November of that year.”
Run 2 Rebuild recruits men at the JHM for a month-long running commitment. Each person enrolled in Run 2 Rebuild is asked to dedicate two mornings a week to run with the group. Harris explains that a few men enrolled in theinitial month-long program have continued running with the group after they completed their first month. “As of October, we have had over thirty-five runners from Jimmie Hale Mission,” he explains. “The current volunteer base is over twenty men who commit to run one morning per week. Morning volunteer shifts can vary but we try to have at least one volunteer per runner.”
The 1:1 ratio helps establish community and build relationships within the group, which is a main priority for the organization. The group currently has seven runners from JHM committed for the month of November.
 R2R client George Campbell runs with MS3 James Harris.Jackson Harbarger, a student in the UAB School of Dentistry, stepped up to help lead the group and serves as the program launch coordinator when new runners begin each month.
R2R client George Campbell runs with MS3 James Harris.Jackson Harbarger, a student in the UAB School of Dentistry, stepped up to help lead the group and serves as the program launch coordinator when new runners begin each month.
The group makes it a priority to acknowledge and celebrate when participants achieve running milestones, like 10, 25, or 50 total miles. Current scientific studies published in PLoS One and by the American Psychological Association are exploring the relationship between encouragement, motivation, and success—hypothesizing that encouragement and motivation solicit long-lasting brain emotional responses.
Run 2 Rebuild uses “Miles Further” boards for clients to sign to recognize when they hit a certain cumulative distance and to track milestones. “It is very rewarding to watch these men progress throughout the month. We ask them to set goals at the beginning and we make sure to celebrate each goal accomplished, encouraging them to continue setting higher goals,” Harris explains.
Several local businesses and individuals have donated goods and services to the group. Harris says those donors have helped make the program a reality.
For example, the running goods store The Trak Shak donated shoes to the clients, so that a lack of running shoes is not a concern. Mel Cosio, P.T., DPT, a recent graduate from the UAB Physical Therapy program, designed a full stretching routine for JHM clients to follow. “We go through this routine each morning before we run to prevent injuries and establish healthy habits,” Harris says. Also, UAB Medicine’s Sports and Exercise Medicine Clinic has provided new running shirts for the group to wear as they participate in races around the community.
Harris, who has an early interest in surgery, says this project has provided immense fulfillment in both his academic career and his personal life. “Building relationships with these men and providing support and motivation have been our goals from day one. I have been extremely blessed with the new friendships that I have formed through this program.”
“Many of these men have incredible stories and it is amazing to hear them open up and share great memories, struggles, and everything in between with us during our runs. My fulfillment comes from knowing that I can play a small role in helping these men achieve their goals and then use the traits that they develop through running to enhance other areas of their lives.” – Mary Ashley Canevaro
A Passion for Wellness: Lauren Nassetta supports faculty and trainees as Professional Development Office director
When it comes to knowing what you want to do for a living, Lauren Nassetta, M.D., is one of the lucky ones. When she was only 4 years old, Nassetta confidently declared to her mother that one day she would become a pediatrician. And that is exactly what happened after Nassetta graduated from the UAB Heersink School of Medicine in 2006.
Life and learning don’t always follow such a well-planned path, and numerous obstacles can crop up along the way, especially in the fast-paced and ever-changing field of medicine. As the new director of the Heersink School of Medicine’s Professional Development Office, Nassetta’s goal is to help level out what she calls “rough patches.”
“We won’t be able to completely smooth it over for you,” Nassetta says, “but we can provide support and encouragement to help you get through it. That’s a role that we serve.”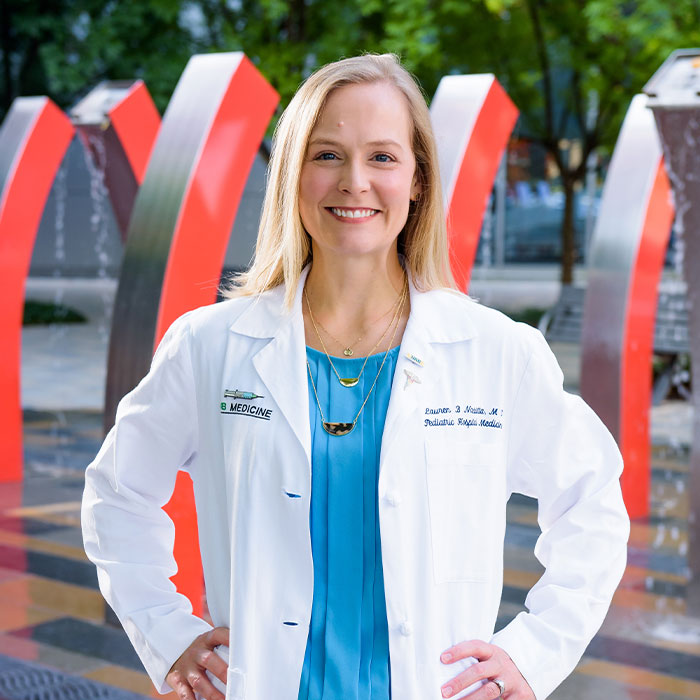 Nassetta says she loves working with her team because of the "passion and compassion with which they are approaching this role of maintaining wellness."
Nassetta says she loves working with her team because of the "passion and compassion with which they are approaching this role of maintaining wellness."
It is a role that has long intrigued Nassetta, even as she never lost sight of her childhood dream of pediatrics. A native of Atlanta, Nassetta moved to Birmingham in 1997 to attend Birmingham-Southern College (BSC), where she majored in biology-psychology.
“I’ve always been interested in how people think and learn, which ties in with overall wellness,” Nassetta says. “I’m not a psychologist by any means, but I’ve always been curious about what makes people behave in certain ways and about how our past experiences impact how we interact with one another and the world around us.”
After graduating from BSC, Nassetta completed medical school, Pediatrics residency, and a chief resident year at UAB. She is an associate professor in the Division of Pediatric Hospital Medicine in the Department of Pediatrics, where she serves as an associate residency program director and the chief wellness officer.
It was during a medical conference she attended while serving as co-director of the Pediatrics clerkship that Nassetta first began to consider the importance of wellbeing on learning. A fellow medical educator presented data about burnout and depression among students and the impact it had on their education and patient care. Importantly, he also showed that something could be done about it.
“Basically, how people are feeling directly impacts how they learn and how they function as physicians,” Nassetta says. “It was a really powerful talk. From that I started to get interested in burnout in residency and medical students—what to do about it and how to prevent it.”
Nassetta began directly confronting such issues as the UAB site principal investigator for the national consortium studying burnout and resilience in pediatrics residents. She will expand that mission in her role at PDO, where she is joined by a team of physicians, psychologists, and counselors.
“What’s really exciting is the opportunity to work with people who are also excited about doing this same work,” Nassetta says. “I love the team I’m working with and their enthusiasm, the passion and compassion with which they are approaching this role of maintaining wellness. It’s an awesome opportunity to make sure that UAB is a place where people can feel good at work.
“Our goals are to expand our outreach and our resources, in order to increase the number of people we can help support. We want to be more of an obvious presence on campus.”
To accomplish these goals, Nassetta says the PDO is working closely with a variety of entities, including the UAB Heersink School of Medicine, the Office of Graduate Medical Education, the Employees Assistance and Counseling Center, the Department of Psychiatry and Behavioral Neurobiology, and Student Health Services.
“People can always come to us for assistance, but we also want to interact with any of the other groups that are doing some of the same type of work on campus,” Nassetta says. “We want to be an immediately accessible place for people to start with when they’re in distress. Just a safe place where you can go when you’re having a rough patch and need somebody to talk to.
“I want to make sure that the Heersink School of Medicine and UAB Medicine are places where people can continue to grow, feel supported, and find meaning. The role of PDO within that is to care for the whole by caring for individuals. It is our mission to equip, encourage, and empower the people of UAB so that everyone can thrive at work.” – Cary Estes
From Africa to Alabama (and Back Again): Grant leverages “reverse innovation” to reduce alcohol abuse and improve HIV outcomes abroad and at home
At first glance, there may appear to be few similarities between Zambia, a landlocked country in southern Africa, and rural Alabama. Apart from the 8,000 miles of land and sea between them, however, the two regions both grapple with longstanding HIV epidemics, widespread poverty, and significant barriers to accessing medical care and public health services. Another similarity is the prevalence of alcohol use disorders, substance use disorders, and mental health conditions, all of which can contribute to the spread of HIV.
A five-year, more than $5.8 million P01 (program project) grant awarded to the UAB Marnix E. Heersink School of Medicine from the NIH National Institute on Alcohol Abuse and Alcoholism is funding an innovative series of projects to address these concerns in both Zambia and rural Alabama. Critically, it adapts interventions and strategies that have been proved in one setting to the other. Karen Cropsey is the Conatser Turner Endowed Professor of Psychiatry in UAB’s Department of Psychiatry and Behavioral Neurobiology and co-director of the Center for Addiction and Pain Prevention and Intervention at UAB.
Karen Cropsey is the Conatser Turner Endowed Professor of Psychiatry in UAB’s Department of Psychiatry and Behavioral Neurobiology and co-director of the Center for Addiction and Pain Prevention and Intervention at UAB.
“This is tech transfer—we are exchanging the best of our practices,” says Karen Cropsey, Psy.D., Conatser Turner Endowed Professor of Psychiatry in UAB’s Department of Psychiatry and Behavioral Neurobiology and co-director of the Center for Addiction and Pain Prevention and Intervention at UAB. “We are adapting a proven therapy from Zambia to Alabama called the Common Elements Treatment Approach, or CETA, and taking our success with patient-reported outcomes from Alabama to Zambia.”
Cropsey is one of the principal investigators for the overall Zambia Alabama HIV Alcohol Comorbidities Program, known as ZAMBAMA, along with Michael Vinikoor, M.D., associate professor in the UAB Division of Infectious Diseases.
ZAMBAMA contains two separate but related projects. Both rely on the Common Elements Treatment Approach, or CETA, a proven, peer-led program of cognitive behavioral therapy originally developed at Johns Hopkins University. CETA combines elements common to effective treatments for problems such as depression and trauma into a single treatment model that can be delivered by trained laypeople. CETA has demonstrated effectiveness in countries from Iraq and Thailand to Zambia, Ethiopia and Myanmar.
“Most therapies are single-diagnosis-focused—just substance use, just depression, etc.,” Vinikoor says. “Therefore, having a single treatment model that caters to a range of symptoms and complex cases reduces the costs of training and time and the need to refer patients to specialty care.”
The project also expands a longstanding collaboration between UAB and the Centre for Infectious Disease Research in Zambia, a Zambian non-governmental institution with an operating budget of more than $40 million per year. Three UAB Heersink School of Medicine faculty are embedded full-time with CIDRZ, including Vinikoor, Carolyn Bolton Moore, MBBS, associate professor of Medicine, and Albert Manasyan, M.D., assistant professor of Pediatrics.
“The collaboration puts UAB experts on the ground in Zambia to strengthen research and public health capacity and address major global health challenges,” Vinikoor says. “Such collaborations are what make UAB a leading U.S. university in global health. In addition to ZAMBAMA, the UAB-CIDRZ team is implementing research focused on a range of conditions, including COVID-19, HIV prevention, maternal and newborn health, cervical cancer, and viral hepatitis. The collaboration also creates opportunities for UAB students and trainees interested in international health to travel to Zambia for a rotations, internships, etc.”
For the ZAMBAMA project, CIDRZ researchers, including social scientist Anjali Sharma, Ph.D., biostatistician Samuel Bosomprah, Ph.D., and infectious diseases expert Izukanji Sikazwe, MBChB, will share with UAB their expertise in integration of CETA into the HIV health system, Vinikoor says.
This will not be the first time that public health lessons learned in sub-Saharan Africa will be translated back to Alabama, Vinikoor adds. In the Finding Respect and Ending Stigma around HIV, or FRESH, study, Janet Turan, Ph.D., professor in the Department of Health Behavior, and Scott Batey, Ph.D., associate professor in the Department of Sociology, implemented a program to reduce HIV stigma among health workers in Alabama that was adapted from Turan’s earlier research in Kenya. “UAB’s global health work impacts not only populations in low- and middle-income countries, but also communities back home in Alabama,” Vinikoor says.
Alcohol consumption is rising in sub-Saharan Africa and, especially since the beginning of the COVID pandemic, in rural Alabama, the researchers point out. And unhealthy alcohol use is often complicated by comorbid mental illness and/or other substance use, they say. 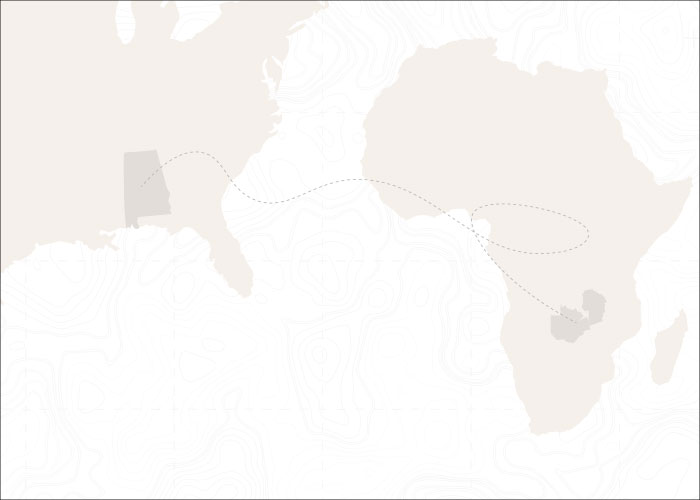 Rural Alabama and Zambia grapple with many of the same health challenges, making effective solutions transferable between the two.
Rural Alabama and Zambia grapple with many of the same health challenges, making effective solutions transferable between the two.
What is the link between alcohol use and HIV? Research has demonstrated that alcohol use disorders (and mental health problems) contribute to risky behaviors that may expose a person to becoming infected with HIV. In those living with HIV, drinking is associated with delays in learning one’s status through HIV testing, lower engagement in care and treatment, and lower adherence to lifesaving antiretroviral medications. As measured by blood tests, people with unhealthy alcohol use also are less likely to have achieved viral suppression, which makes them more likely to transmit the virus to others. Finally, some data suggest that people with HIV may be more sensitive to the effects of alcohol than those without it.
The Zambia-based project, with Vinikoor as MPI together with Jeremy Kane, Ph.D., from Columbia University, will evaluate the effectiveness, including cost-effectiveness, of implementing CETA and another alcohol-reduction intervention known as a brief alcohol intervention.
It also will utilize patient-reported outcomes, or PROs, in Zambian clinics, learning from UAB’s expertise. PROs, implemented as quick surveys of patients during each clinic visit, have been used successfully at UAB’s 1917 HIV/AIDS Clinic for several years to identify patients with unmet mental health or substance-use concerns. “The patients answer questions about depression, alcohol use, medication adherence, and more,” Cropsey says.
The Alabama project will use telemedicine to implement CETA in rural Ryan White HIV clinics across the state. “This is what we call ‘reverse innovation,’ taking a success from low-resource settings in a developing country and figuring out what lessons we can apply here in Alabama,” says Ellen Eaton, M.D., assistant professor in the UAB Division of Infectious Diseases. Eaton is MPI for the Alabama project, as is Cropsey.
There is a nationwide shortage of clinical psychologists, Cropsey points out, so approaches such as CETA have great promise. For the Alabama project, the intervention will be delivered remotely from Birmingham using clinical psychology graduate students from the UAB College of Arts and Sciences. “Using telemedicine makes this more translatable to a wider variety of settings,” Cropsey says. – Matt Windsor
The Write Stuff: Otolaryngologist Kirk Withrow creates fictional worlds rooted in science
Despite his busy schedule as an associate professor in the Department of Otolaryngology, Kirk Withrow, M.D., is the author of numerous books and short stories, many with a dystopian slant. His earliest novel, Four, is a psychological/military/medical thriller about a former soldier suffering from PTSD. The Redivivus Trilogy—Threnody, Riposte, and Miasma—is a postapocalyptic survival horror series about humanity’s battle against a deadly pathogen. His most recent novel, Fun World, is set in a fictional theme park where a family must fight to survive amid a zombie apocalypse. Kirk Withrow’s books are available for purchase on Amazon
Kirk Withrow’s books are available for purchase on Amazon
What sets his writing apart is the influence of his medical training, which gives his works a grounding in science despite the often fantastical subject matter. “The whole idea of an apocalypse is an interesting tool because you can pare your characters down to just a few people. And, if you take all the societal rules away, you can explore the extremes of human behavior—you can see the absolute best and the absolute worst in people.”
A friend’s casual question sparked Withrow’s interest in crafting zombie/survival fiction. “Around the time The Walking Dead was coming out, he asked me if there was any way a zombie could ever actually exist. And I was like, ‘Well, no,’ but it got me thinking of aspects of real medical conditions that you could combine that could add up to something like that.
“For instance, there are hormones that control satiety, there are hormones that allow you to sleep or stay awake, there are rare medical conditions where people can’t feel pain. If you think of the prototypical zombie—they don’t sleep, all they want to do is eat, they have uncontrolled aggression, they don’t feel pain—and if you look at it without too much scrutiny, you could see elements of those real medical conditions coming together in something like that. So that’s probably the best way to describe what I try to do with my writing: take bits and pieces of actual science and put them together in a way that, while it’s fiction, there’s a scientific basis behind it.” – Jane Longshore