
Once a year, when Gabrielle Rocque, M.D., an associate professor in the Division of Hematology and Oncology, enters the Kirklin Clinic on the night of the annual ArtBLINK gala, she sees the space where she normally cares for breast-cancer patients reimagined as the site of a lively, black-tie celebration. “It blows me away,” she said. “It’s completely transformed.”
While ArtBLINK has been a successful fundraiser for the O’Neal Comprehensive Cancer Center at UAB for decades, in 2024 it reached a new milestone: for the first time, the event raised more than $1 million. ArtBLINK has become one of the city’s most iconic events, bringing people together to toast the O’Neal Comprehensive Cancer Center and its more than half century of world-class cancer care, research, and innovation. Along with its unique hosting site—the workspace on a normal day for hundreds of physicians in nearly three dozen specialties—the gala stands out for many reasons. As guests enjoy dinner, cocktails, live music, and dancing, local artists are on hand to create one-of-a-kind works of art. Guests begin bidding on the pieces before they are completed.
The enthusiasm surrounding ArtBLINK is emblematic of what the O’Neal Comprehensive Cancer Center means to the people of Alabama and beyond. “The O’Neal Care Center provides our community with access to the best, most cutting-edge care,” said Laura McDonald, president of the O’Neal Comprehensive Cancer Center Advisory Board, which raises money, promotes awareness, and provides support in other important ways. She said part of her own passion for the cause stems from a personal experience with the O’Neal Comprehensive Cancer Center, when her late mother, Karen York, was treated for ovarian cancer about 30 years ago. “I can’t imagine her having received better treatment anywhere else in Alabama,” she said. “I want the same for everybody across the state.”
This year also included a special tribute to Allene and Foots Parnell, who were recognized as the 2024 Director’s Circle honorees for their commitment to the O’Neal Comprehensive Cancer Center. Like McDonald, the Parnells also have a personal connection to cancer, having lost their 22-year-old daughter, Carleton, to the disease. “The Parnells are a great representation of the heart of the advisory board,” McDonald said. “They have spent a good part of their personal lives working to make a difference in cancer-related causes.”

Recognized as among the country’s leading cancer-research institutions, the O’Neal Comprehensive Cancer Center was one of the first eight facilities in the nation to receive the Comprehensive Cancer Center designation from the National Cancer Institute (NCI). It remains the only such center in Alabama.
Barry Sleckman, M.D., Ph.D., director of the O’Neal Comprehensive Cancer Center and holder of the Evalina B. Spencer Chair in Oncology, said money raised by ArtBLINK is earmarked for the center’s pilot grant program. In his four-year tenure, more than 60 pilot grants have been funded. “When we solicit funding proposals, we don’t indicate any particular type of work or type of cancer that we want to fund,” Sleckman said. “We simply say, ‘We want really great ideas that are relevant to cancer.’” These range from laboratory research to population research and what Sleckman identified as “translational trials—taking discoveries that are either made here or potentially elsewhere and planning for testing those discoveries in people with cancer.”
Rocque’s work represents the kind of forward-thinking research that benefits from the pilot grant program. In addition to caring for breast-cancer patients in the clinic once a week, she is deeply engaged in research that focuses on a broader picture of cancer care. “Much of the research I pursue is in communication, patient experience, and quality of life,” Rocque said. This includes shared decision-making, which focuses on including patients’ personal needs and values as part of the treatment-formation process; patient-reported outcomes, in which information directly reported by patients about their health status is integrated into their care; and addressing what she calls the “financial toxicity” of cancer and finding ways to mitigate the financial hardships that often come with a cancer diagnosis.
“We’re just scratching the surface of the power of bringing patient voice more purposefully into cancer care and delivery,” she said.
Rocque calls ArtBLINK her favorite event of the year. “It’s such a great opportunity to celebrate and be thankful,” she said, adding that while she’s never had the winning bid on an artwork produced at the event, she has commissioned pieces from the featured artists afterward. (One of these, a smaller-scale version of a painting from ArtBLINK, hangs in her office.) “There’s something valuable and important in my mind about having this event in a place where we care for people, and it’s a great way for the community and providers at UAB to intermix and get to know each other a little bit outside of the clinical setting. I don’t know of many other occasions where that happens in such a fun way.”
-Rosalind Fournier
To learn more about giving to support the O’Neal Comprehensive Cancer Center at UAB, contact Senior Director of Development Lisa Roth at 205-934-0930 or leroth@uabmc.edu.

A distinguished professor in the Heersink School of Medicine, a professor in the Department of Surgery, and holder of the Champ Lyons Endowed Chair in General Surgery, Aurelio Galli, Ph.D., D.S.c, was introduced to martial arts at age 6, when his father enrolled him in judo to manage his frequent falls. Growing up in northern Italy, Aurelio swiftly excelled, becoming a multiple-time regional champion and achieving a brown belt.
Despite his early success, Galli’s judo career faced an abrupt halt due to a medical condition. "I had to quit when I went for a competitive screening in Italy because they found out I was myopic and were concerned about retinal detachment," he explained.
Years later, it was his daughter who steered him towards Brazilian jiu-jitsu (BJJ). "Around the time of COVID, my daughter suggested I try a Brazilian jiu-jitsu place she saw," Galli shared. He soon found himself drawn back to the competitive arena and began to train more consistently and compete regularly about a year and a half ago.
Balancing his professional responsibilities with his training is no small feat for Galli. "When I don't have grants, I try to train as much as I can. My gym, SBG Spartan Academy, is open every day except Sunday," he explained.
Competing in BJJ has brought Galli both recognition and personal satisfaction. "This year, I competed in the Pan American and won, which is one of the top three competitions," he said. His dedication saw him place first several times in the Nashville and Atlanta Opens and he placed second in an open weight category in Atlanta, even while battling an injury.
The sport has not only been a physical outlet but also a source of camaraderie and community for Galli. "Brazilian jiu-jitsu is very relaxing and excellent for cardiovascular health. The community is welcoming and nonjudgmental, which I appreciate," he shared.
This inclusive environment is one of the many reasons he recommends BJJ to others. "It's an incredible sport, great for fitness and self-defense, especially for smaller individuals," Galli said.
Galli reflects on his current standings with pride. "As a master competitor, I'm currently ranked number two in my weight and belt division and number 19 overall across all weight divisions," he shared. For Galli, BJJ is more than just a sport. "I think Brazilian jiu-jitsu offers various levels of engagement, from casual to competitive. It's less about winning and more about mutual respect and personal growth," Galli said.
-Kayla Gibson
Families of children with autism spectrum disorder (ASD) face complex and often overwhelming challenges—understanding how the condition impacts their child, accessing support services, and coping with the financial strain of therapies and interventions that health insurance may not cover. Birmingham business owner and CEO Sheila Benson and her family experienced many of these struggles when her grandson, now 16, was diagnosed with ASD at age 2. “It was difficult for my son’s family to access the appropriate resources and therapies that my grandson, who is nonverbal, needed after his ASD diagnosis,” she explained. “Waiting lists sometimes caused a two-year gap in obtaining a therapy that he needed, which caused stress and frustration for our family. Also, insurance didn’t pay for his therapies at that time.” Benson said several friends and their families have also struggled to cope with the challenges of a child’s ASD diagnosis. “Seeing these difficulties within my own family, as well as those experienced by others, made me more aware of what individuals with ASD and their families need,” she said.
ASD is a lifelong neurological and developmental disorder that affects how people interact with others, communicate, learn, and behave. Statistics from the Centers for Disease Control and Prevention show the prevalence of ASD is significant and increasing, with one in 36 children diagnosed in 2023 compared to one in 44 only two years earlier.
Benson explained that her desire to support individuals in the ASD community was the catalyst for establishing a philanthropic partnership with the UAB Civitan-Sparks Clinics, which provide evaluation and intervention services for those with physical, developmental, learning, and behavioral challenges. The clinics, including the UAB Autism Spectrum Disorders Clinic, are part of the Civitan International Research Center (CIRC), an interdisciplinary hub focused on service, education, and research for neurodevelopmental disorders. “Through my partnership with UAB, I’m focused on helping other families of children with ASD connect with the resources they need and advancing research that can help those with ASD have the best possible future,” said Benson. “If we can get people with ASD diagnosed early and connect them to resources and effective therapies, they can live more functional lives and reach their full potential.”
Laura McGuinn, M.D., clinical director of the UAB Civitan-Sparks Clinics and director of the UAB Division of Developmental and Behavioral Pediatrics, said research shows that early intervention for children with ASD leads to greater improvements in communication, behavior, and mental health when compared to children who begin interventions later. “Ms. Benson’s generous partnership has been invaluable in helping us to enhance our care coordination support infrastructure to connect newly diagnosed patients to resources and interventions more quickly,” she explained. “Bridging this gap from diagnosis to intervention helps give children with ASD the best chance to achieve optimal outcomes and reduces the stress and uncertainty many families feel after a diagnosis.”
As part of the clinic’s care coordination, social workers conduct regular check-in calls with families after diagnosis to ensure connection to therapies and referrals to community-based resources. “Ms. Benson’s support has allowed us to add social work personnel, who have made more than 3,000 check-in calls with newly diagnosed families during the past year,” said McGuinn, holder of the Thomas H. Lowder Endowed Chair in Developmental and Behavioral Pediatrics. “Much of our previous follow-up was done by a physician or psychologist, which displaced the time we could spend diagnosing patients. We now can complete more diagnostic evaluations because of the additional social work personnel.”
The additional personnel also has enabled the clinic to collect vital data that identify outcomes related to the needs addressed during check-in calls and to document the impact of these efforts for hospital administrators, state policy-making agencies, and other stakeholders. “These data will help to define and shape a standard of care for the future,” said McGuinn. Benson’s gift also has funded the development of an upcoming interactive website that will streamline statewide resources into an accessible, time-saving source for families and referring providers. “Many of these resources are fragmented, so developing a user-friendly source of this information can improve access to care and lower stress for families,” McGuinn explained.
Benson’s philanthropic partnership also has been instrumental in advancing critical research focused on identifying effective interventions to improve the lives of people with ASD and their families. “Philanthropic partners like Ms. Benson are essential to driving new ideas and bold experimentation in ASD and other neurodevelopmental disorders,” explained Craig Powell, M.D., Ph.D., director of the Civitan International Research Center and the Virginia B. Spencer Endowed Chair in the UAB Department of Neurobiology. Powell said more than 100 scientists in the UAB Civitan International Research Center for Neurodevelopmental Disorders are engaged in research to develop evidence-driven therapies for ASD-related symptoms, including sleep challenges, with a goal to study all symptom domains, such as anxiety and obsessive-compulsive disorder (OCD)-like behaviors. “Early-stage therapeutic research often is not funded by traditional mechanisms such as the National Institutes of Health,” Powell said. “Philanthropic support allows our scientists the freedom to explore novel ideas and approaches, generating data that can be leveraged to obtain larger grant funds to bring these ideas across the finish line—impacting patients and their families for decades to come.”
“The work Dr. McGuinn, Dr. Powell, and other UAB clinicians and researchers are doing is priceless,” said Benson. “They give so much of themselves and understand the challenges for people with ASD and their families.” Benson’s grandson, now in high school, recently attended the prom for special needs students and is learning life skills. “We’re grateful for his progress, understanding that ASD is a lifelong condition with continued challenges,” she said. “I want people with ASD and their families to know they’re not walking this road alone—there are resources available with compassionate experts to provide support and help as they navigate this unfamiliar journey.”
-Yolanda Heiberger
Throughout her career as a young physician, the late Priya Nagar, M.D., had a special understanding of her patients’ challenges because of her own experiences with pain, serious illness, and healing. Priya was diagnosed at age 9 with chronic kidney disease (CKD) and kidney failure in her native India and underwent a kidney transplant when she was 14, with her mother as her living donor. The transplant allowed Priya to pursue her dreams of becoming a doctor after her family’s move to the United States. She enjoyed a rewarding career as a hospitalist at Baptist Medical Center in Montgomery, where she completed her residency in family medicine. “Priya had such tremendous doctors her whole life and was inspired by their work,” said her younger sister, Anusuiya Nagar, M.D.
In 2017, at the age of 36, Priya lost her battle with a rare form of lymphoma, a complication of long-term immunotherapy for her CKD and previous kidney transplant. “Priya’s treatment involved chemotherapy, losing her hair, and other challenges,” recalled Vineeta Kumar, M.D., a professor in the Heersink School of Medicine and holder of the Robert C. and Cutessa D. Bourge Endowed Professorship in Transplant Nephrology, who was part of Priya’s medical team at UAB. “As a patient, she channeled her energy into being a positive presence for everyone around her.”
After Priya’s untimely passing, her parents, Rajinder and Kamaljeet Nagar, and sister, Anusuiya, wanted to honor Priya’s incredible life of gratitude and legacy of caring for others. “In the aftermath of her loss, we had energy that was uncomfortable and unwelcome,” explained Anusuiya, who serves as program director for the Adult Psychiatry Residency Program at the University of South Carolina School of Medicine. “We had a painful void that we could either leave empty or fill with something meaningful.” The family established the Priya Nagar, M.D., Foundation in 2018 to support promising research to understand the underlying causes of CKD and reduce its prevalence.
Because Priya received excellent care from providers in the UAB Division of Nephrology, the family chose UAB as the primary recipient of the foundation’s funds. “Priya had a team of nephrologists at UAB, and they were a second family to her and to us,” Rajinder Nagar said, adding that nephrologist Anupam Agarwal, M.D., senior vice president for Medicine and dean of the Heersink School of Medicine, Kelly Hyndman, Ph.D., associate professor in the UAB Division of Nephrology, and Kumar were instrumental in introducing them to UAB’s innovative kidney disease research. “The human story behind the Nagar family’s effort was powerful and humbling,” Kumar recalled.
The family’s fundraising efforts for the foundation were spearheaded by Kamaljeet Nagar, affectionately known as Bubby, who began selling her hand-knitted, woolen dog sweaters on the foundation’s website. An annual 3K walk in Naperville, Illinois, where the family lived for many years, also generates funds for the foundation. One of the most popular fundraising events is an annual neighborhood dinner that Kamaljeet hosts in Greenville, South Carolina, where the couple retired in 2021.
“She prepares and serves delicious, homemade Indian food on white tablecloths to our guests,” Anusuiya describes. “The event began with 22 people, and this October, our fourth year, we anticipate more than 100 people.”
Through the Nagar family’s extraordinary efforts, the foundation has made significant annual gifts to the UAB Division of Nephrology to advance novel, promising research that could help to prevent CKD and lead to more effective treatments. Hyndman shared that the Dr. Priya Nagar Pilot Award she received from the foundation was pivotal in achieving early research results that led to an R01 grant from the National Institutes of Health. “Pilot awards allow investigators to generate preliminary, published data that can help to secure a larger grant, such as an R01, to continue their research,” she explained. Hyndman studies how proteins called histone deacetylases (HDACs), which regulate gene function in cells, could be manipulated to treat acute kidney injury. “The pilot award allowed me to use cutting-edge technology to produce data from which I’m still generating new hypotheses,” she said.
The foundation has also provided funds through the Priya Nagar, M.D., Innovation Award to two UAB investigators who have each developed novel medical devices with potential to treat CKD-related conditions. “The incredible generosity of Dr. Nagar’s family has been transformational in helping to fund cutting-edge research that will result in the development of new therapies for kidney disease,” said Orlando Gutierrez, M.D., director of the UAB Division of Nephrology and holder of the Marie S. Ingalls Endowed Chair in Nephrology Leadership. “We are humbled to honor Dr. Nagar’s memory in this way, establishing a permanent legacy for her that will help thousands of individuals with kidney disease and related ailments well into the future.”
Anusuiya said the foundation’s mission reflects the gratitude that defines Priya’s legacy. “Despite her serious health challenges, Priya remained grateful for the gift of time the kidney transplant gave her, especially the opportunity to become a doctor and care for patients,” she said. Rajinder Nagar recalled of Priya, “I often found her late in the evening talking to the family of a patient. This is the kind of dedicated physician she was.” Kumar says that Priya’s essence was to do all she could to make others’ lives better, adding, “Through research funded by the foundation established in her name, Priya’s legacy of giving and gratitude continues, with the potential to transform countless lives.”
-Yolanda Heiberger
Growing up in Eutaw, Alabama, (pop. 2,803), Drake Lavender, M.D., suffered from asthma and severe allergies. His lifeline was his family doctor, Rucker Staggers, M.D., who treated him weekly with allergy shots, and the two developed a strong patient-doctor bond.
“He became a mentor for me,” Lavender said. “I didn’t know I wanted to be a family medicine physician but I knew I wanted to be like Dr. Staggers. I wanted to have that kind of impact on someone’s life.”
Today, as director of Rural Programs at the University of Alabama (UA) College of Community Health Sciences (CCHS), Lavender is acutely aware of what he didn’t know as a kid—that primary care physicians like Staggers are increasingly rare in small towns like Eutaw.

According to the Alabama Office of Healthcare Workforce (AOHW), 52 rural population centers in the state have a shortage of primary care physicians. The repercussions for these medically underserved communities are dire. A 2021 National Center for Health Statistics (NCHS) brief stated that from 1999 to 2019, differences between rural and urban areas in death rates for conditions like heart disease, cancer, and chronic lower respiratory disease widened. In 2019, the age-adjusted death rate in rural areas was 20 percent higher than in urban areas.
The University of Alabama System launched Rural Programs in the 1990s in response to these alarming statistics. It’s an umbrella program designed to recruit potential medical students from rural Alabama in hopes they will go back to serve these communities where they are desperately needed.
Lavender himself became one of these students in 1996 when he joined the first cohort of Rural Medical Scholars, a subset of Rural Programs that represents a joint effort between the Heersink School of Medicine and CCHS. Rural Medical Scholars recruits college students who want to attend medical school and, it is hoped, practice in rural Alabama counties. After graduating from medical school at UAB, with his clinical years spent in Tuscaloosa, he completed his residency and served as chief resident at The University of Alabama Family Medicine Residency. Lavender then began practicing primary care in Gordo, Alabama (population 1,584).
In Gordo, Lavender realized how much he liked practicing in a rural setting. “I enjoyed the life of a small town and the closeness you can have with your patients,” he said. “They aren’t just your patients in the office. They are your friends at the grocery store, at church, at football games. I grew up in that kind of community and it appealed to me.”
In 2014, he decided to return to UA and later took over as director of Rural Programs. “It’s come full circle for me to return to the program that gave me my chance,” he said. “I can help other people get a chance, too.”
Lavender said recruiting rural students into medicine requires changing established norms. “While the data tells us the people most likely to practice in rural areas are those who come from rural communities,” he said, “our country’s medical education system has mostly failed at recruiting and admitting people from rural areas.” Lavender points to a study by Scott Shipman, M.D., MPH, the director of primary care initiatives and clinical innovations at the Association of American Medical Colleges (AAMC), finding that students from rural backgrounds made up just 4.3 percent of the country’s incoming medical student body. “That’s a big problem if you’re trying to get people to practice in rural areas. You really need physicians who understand rural culture and are comfortable living and practicing in those communities.”
Rural Programs includes several pathways for students to become exposed to and enter the medical and health care fields. Rural Medical Scholars—the program through which Lavender came—is just one. Others include Rural Health Scholars, in which high-school students spend part of a summer on the UA campus, take classes, and learn about careers in medicine. Another program, the Tuscaloosa Rural Premedical Internship, invites undergraduates to shadow local preceptors in Tuscaloosa and small towns around the state. Minority Rural Health Scholars targets high school graduates from communities traditionally underrepresented in medicine. And this past year saw the launch of Rural Dental Scholars, affiliated with the UAB School of Dentistry.
Lavender spoke about Rural Programs at the 2023 Medical Alumni Weekend and was encouraged by the reception. “A lot of medical alumni members were very interested in what we’re doing and how we can continue to work on this issue,” he said. “The focus on primary care and rural health needs to be at the forefront in all of our medical schools.”
Just as the problem has been growing over time, Lavender adds, it will take continued effort to reverse it. “As of this year, we have 58 full-time, primary care physicians in rural Alabama who’ve come through the Rural Medical Scholars Program,” he said. “In addition to all their great work as doctors, we ask them to help us find the next generation. They have a wonderful platform to help us identify students in their communities to send back to our program and start the cycle over again.”
-Rosalind Fournier
There is an open secret among tattoo artists, dermatologists, and the small group of researchers studying the effects of tattoo ink: Red ink causes the most problems.
These problems include rashes—itchy, sometimes painful, and occasionally disfiguring—and pseudolymphomas—benign swellings around lymph nodes that resemble cancers of the lymph system. Both rashes and pseudolymphomas are symptoms of an allergic reaction. While these problems are not unique to red ink, red is the most likely culprit. One student from the Heersink School of Medicine launched a mission to understand why.
Doctors are more likely to see tattoo complications now than ever before. Thirty percent of Americans have at least one tattoo, up from 21 percent in 2012, according to a 2019 poll. A separate study in 2017 estimated the range of post-tattoo complications at anywhere from 2 percent to 30 percent; in that paper’s review of patient cases in Finland, 75 percent of allergic reactions were against the red color.
Until the mid-20th century, the reason for red’s ravages was clear: Red tattoo inks often contained mercury. But as the adverse effects of mercury and other metals became widely known, tattoo artists avoided these inks and manufacturers turned to alternative formulas. Today, manufacturers have largely switched to inks colored by organic compounds instead of compounds including heavy metals, and recent studies have found low concentrations of mercury in commercial inks. But red ink is still the most likely color to cause skin problems.
Tiffany Mayo, M.D., associate professor and director of the UAB Department of Dermatology Clinical Research Unit, discussed this puzzle during a student lecture in 2022. Her description and slides immediately caught the attention of then-third-year medical student Matthew Kiszla, the son of an artist and an artist himself who had cheekily listed a book that he and his mother illustrated among the publications on his medical school application.

“I am a very visual person,” Kiszla said, and even though he does not have any tattoos himself, “that attracts me to tattoos and also to dermatology, with its vivid, dramatic rashes.” Plus, Kiszla was an undergraduate chemistry major. The chemical mystery Mayo described was irresistible, he said—“I just had to know why.”
Kiszla’s interest became a passion to understand the effects of tattoo inks on human health and to advocate for increased attention to safety. In February 2023, Kiszla, Mayo, and another professor in the Department of Dermatology, Craig Elmets, M.D., synthesized results from nine recent studies of tattoo inks worldwide in a review article published in the journal Chemosphere. “Unsafe levels of restricted elements”—including chromium, cadmium, barium, arsenic, and zinc—“continue to be detected across studies, warranting further investigation under a regulatory lens,” they wrote.
“Although the United States is the world’s foremost producer of tattoo inks, they are virtually unregulated at a national level,” Kiszla said. “Tattoo inks can be formulated with a wide range of pigments, preservatives, solvents, and other contaminants, which have been associated with rashes that range from transient to disfiguring.”
And there may be other, hidden effects as well. “The potential systemic implications are unknown,” Kiszla said. “While researchers have found that ink can travel from its site of injection via the lymphatic system and be collected into lymph nodes, they have yet to determine whether this concentration of toxins poses any increased risk.”
Kiszla says Europe, the world’s second-largest market for tattoo ink manufacturers, leads the way in terms of research and regulation.
A series of resolutions introduced in Europe starting in 2003 set maximum allowed concentrations for tattoo ink ingredients; in 2022, these guidelines became binding on all members of the European Union. Nearly all research on the chemical makeup of tattoo inks has been done at European universities, Kiszla notes. In their Chemosphere paper, Kiszla, Mayo, and Elmets compared these new European regulations with the concentrations of metals found in tattoo inks as reported in published studies.
Kiszla then turned his attention to organic inks. He wrote a paper on azo dyes with Lauren Kole, M.D., an assistant professor in the UAB Department of Dermatology—who, like Kiszla, holds an undergraduate degree in chemistry. Organic azo dyes are the new standard for tattoo inks as the industry has shifted from metal-based inks. “Warm tones—yellow, orange, and red—have a high concentration of these azo structures,” Kiszla said.
Kiszla said the fact that red inks still cause the most adverse reactions, as they did in the days of mercury, could be a coincidence but there is not yet enough data to be sure. “Ultimately, I hope the studies support the development of safer tattoo inks,” Kiszla said. “My goal is not to impinge on artistic expression but to make body art as safe as possible and as well understood as possible.”
- Matt Windsor
A nationwide study of 196 cities shows that housing discrimination from 90 years ago still casts a shadow of inequities in colon cancer care today, S.M. Qasim Hussaini, M.D., assistant professor in the Division of Hematology and Oncology, and colleagues at the American Cancer Society and Johns Hopkins School of Public Health reported in the journal JCO Oncology Practice.
In the 1930s, the federally sponsored Home Owners’ Loan Corporation, or HOLC, used racial composition to map residential areas worthy of receiving mortgage loans and areas to avoid. Neighborhoods high in Black, immigrant, or minority non-white populations were redlined as hazardous for home loans, creating systemic disinvestment in those neighborhoods, along with wealth inequities and concentration of health-harming exposures and psychosocial stressors. These limitations reduced access to health-promoting goods and resources such as green space, parks, and healthy foods in redlined neighborhoods.
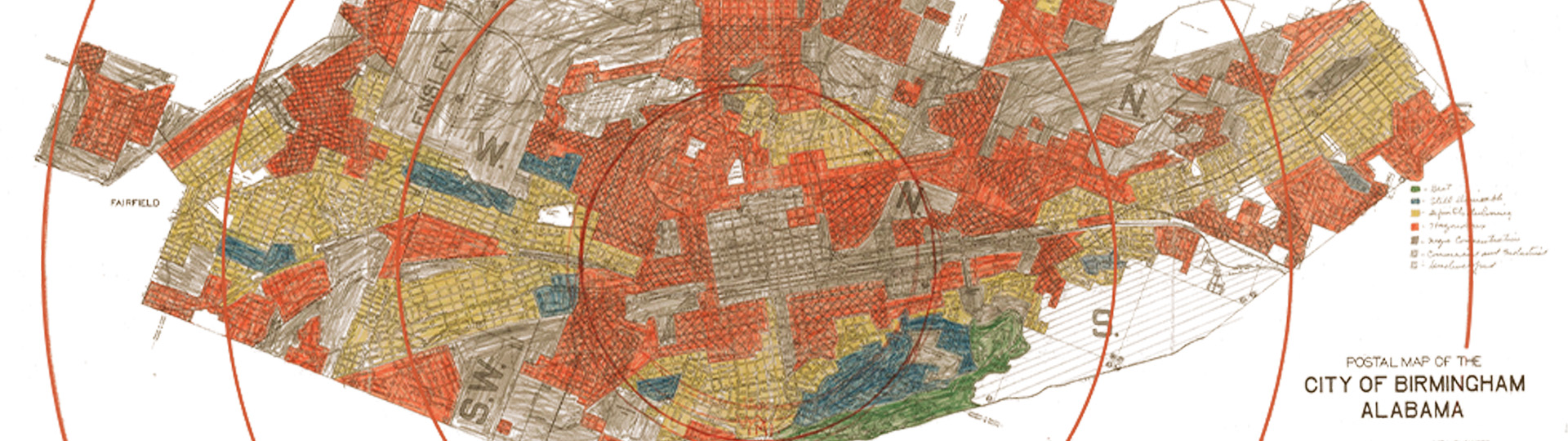
Map showing lending risk "redlining" in Birmingham circa 1933.
To test whether residence in formerly redlined neighborhoods is associated with poorer guideline-concordant cancer care today, Hussaini and colleagues mapped colon cancer care for 149,917 newly diagnosed colon cancer patients from 2007 through 2017, as detailed in the National Cancer Database, against current-day residence in one of the four historical HOLC mapping areas. In the 1930s, the green HOLC areas, or HOLC A, were considered best for mortgage loans; the blue areas, or HOLC B, were considered still desirable; the yellow areas, or HOLC C, were marked as declining; and the red areas, or HOLC D, were flagged as hazardous and to be avoided for mortgage lending purposes.
Overall, the researchers found that individuals diagnosed with colon cancer who resided in previously redlined HOLC D areas across the United States were today more likely to be diagnosed with advanced-stage disease, were less likely to receive guideline-concordant or timely treatment, and had worse survival.
“These findings underscore the long shadow of institutional racism through state- and federal-level discriminatory practices in shaping access to high-quality care and better outcomes for colon cancer, which is amenable to early detection and treatment,” said Hussaini.

S.M. Qasim Hussaini, M.D.
In detail, individuals living in HOLC D areas were more likely to be diagnosed with late-stage colon cancer compared with those living in HOLC A areas. Of the 78,164 people who did not receive guideline-concordant care as defined by the National Comprehensive Cancer Network, the odds of receiving non-guideline concordant care increased for individuals residing in areas with increasing hazard grades assigned by HOLC B, HOLC C, and HOLC D, as compared with individuals residing in HOLC A areas.
Residents of HOLC D areas were 24 percent more likely to not receive guideline-concordant care, 34 percent more likely to not receive surgery, 26 percent more likely to not have at least 12 lymph nodes evaluated during surgery for spread of the cancer, and 20 percent more likely to not receive chemotherapy, compared with people living in HOLC A areas.
A predicted probabilities model—which adjusts estimates of guideline non-concordance for age and sex—showed that non-receipt of guideline-concordant care overall, as well as non-receipt of guideline-concordant surgery, lymph node evaluation, and chemotherapy, sequentially increased from the HOLC A areas through to the HOLC D areas. Compared with those cancer patients living in HOLC A areas, those residing in HOLC B, HOLC C, and HOLC D areas had increased wait times to the start of adjuvant chemotherapy. (Adjuvant chemotherapy is given after surgery in order to kill any remaining cancer cells and reduce the chance of disease recurrence.)
Compared with newly diagnosed colon cancer patients residing in HOLC A areas, those living HOLC C and D areas had 9 percent and 13 percent excess risk of death in statistical models that did not adjust for stage of the cancer at time of diagnosis. After stratification by stage—either early (stages I and II) or advanced (stages III and IV)—the excess risk of death association persisted for the HOLC C and HOLC D areas for both the early and late stages at diagnosis.
Several previous studies by others have noted racial or ethnic disparities in breast cancer outcomes in previously redlined neighborhoods in New Jersey, an increased incidence of advanced-stage lung cancer in formerly redlined areas of Massachusetts, and a lower odds of lung cancer screening for Black individuals in previously redlined areas of Boston. However, those single geographic area studies did not examine whether patients received quality cancer care.
“To our knowledge, this is the first national study, including all states, to evaluate the association between historical institutional racism and current-day receipt of quality cancer care and outcomes using standardized measures of cancer diagnosis, individual and tumor characteristics, receipt of treatment, and survival,” Hussaini said. “Other strengths of the study are a diverse study population including all age and racial groups, and a focus on multiple aspects of care from stage at diagnosis to treatment receipt and survival.”
Colon cancer has about 150,000 new cases each year. It is the third most diagnosed cancer in the United States and the second leading cause of death from cancer, even though colon cancer is amenable to early detection and treatment. Widespread inequities in survival exist due to unequal access to care.
Hussaini’s co-authors in the study, “Association of historical housing discrimination and colon cancer treatment and outcomes in the United States,” are Qinjin Fan, Ph.D., Robin Yabroff, Ph.D., and Leticia Nogueira, Ph.D., of the American Cancer Society, Atlanta, Georgia; and Lauren Barrow and Craig Pollack, M.D., Johns Hopkins University, Baltimore, Maryland.
-Jeff Hanson
It’s been called “The Stethoscope of the Future.” Point-of-care ultrasound (POCUS) can be applied in a variety of settings thanks to its small size and portability, from hospital bedsides to sports sidelines to primary care clinics. These palm-sized devices allow health care providers to quickly and easily perform ultrasound scans, creating detailed images that can help clinicians make informed decisions or provide real-time guidance during a procedure. The devices can aid in identifying various conditions, including soft-tissue infections, fluid accumulation, and heart failure.
In August 2023, the UAB Department of Family and Community Medicine launched an initiative to give every Heersink School of Medicine student across all four of the school’s campuses access to POCUS units, making UAB one of the first medical schools in the United States to provide such access. The initiative was funded with $2 million in federal funds from the department’s Comprehensive Urban Underserved and Rural Experience (CU2RE) program, which is supported by the U.S. Health Resources and Services Administration.
Alabama faces a projected shortage of more than 600 primary care physicians by 2030, and many patients in underserved rural and urban areas already face significant wait times for appointments or have to travel long distances for medical care. Point-of-care ultrasound can play an important role in addressing these shortages by enabling health care providers in resource-strapped areas to conduct ultrasound tests directly in their clinics and quickly get the information they need, instead of requiring the patient to travel to another location or wait for results.

Thanks to the initiative, Heersink medical students will begin learning to use the devices to evaluate every central organ system, diagnose injuries or diseases, and perform procedures. The department will distribute 600 devices for student use and 100 for community preceptors who help train Heersink medical students in their clinics.
“The future of medicine, especially primary care in rural and underserved areas, will require physicians to be nimble, meet patients where they are, and find efficient ways to address a wide variety of concerns right there in clinic,” said Irfan Asif, M.D., chair of the Department of Family and Community Medicine, associate dean for Primary Care and Rural Health, and director of UAB’s primary care service line. “Point-of-care ultrasound offers a great way to do that, especially in rural areas with less access to major hospital systems or other points of care.”
In addition to training students, partnerships with organizations like the Global Ultrasound Institute (GUSI) provide POCUS training for faculty and residents. GUSI provides intensive seminars and skills refinement sessions, ensuring educators can effectively incorporate POCUS into the curriculum.
Since October 2023, the Heersink School of Medicine's Department of Medical Education has hosted several faculty training sessions facilitated by GUSI. In the hands-on sessions, faculty have been able to use POCUS devices on standardized patients and, guided by GUSI staff, see the technology’s impact on patient examination. The events include demonstrations and practice sessions in cardiac, pulmonary, abdominal, vascular, and musculoskeletal imaging. The focus is on simple imaging techniques that allow clinicians to make diagnoses at the bedside that previously would incur the delay and cost of formal imaging. This can be life-saving in emergency or low-resource settings.
According to Senior Associate Dean for Medical Education Craig Hoesley, M.D., “Our mission is to serve the patients of our state, many of whom reside in rural areas and who would benefit from physicians empowered with the training to use this technology effectively. Equipping our faculty and students with this level of knowledge and training is a major step forward for our institution and the physicians we train in accomplishing this goal.”
The CU2RE program is designed to enhance the recruitment, training, and retention of medical students dedicated to serving as family medicine physicians to provide primary care in the medically underserved urban and rural areas of Alabama. The enriched training program addresses six core areas related to interprofessional education, behavioral health, social determinants of health, cultural and linguistic competency, practice transformation, and telehealth. The program has two pathways—Urban Underserved and Rural—for students interested in primary care, health equity, and serving underserved patients.
-Kayla Gibson and Caroline Newman
For a fungus, there is no place like alabama.
“Alabama is a hotbed for fungal diseases,” said Peter Pappas, M.D., professor in the Division of Infectious Diseases in the Heersink School of Medicine. “We see as much or more in the way of fungal infections as anyone in the country.” Pappas is a leader of the Mycoses Study Group, a world-renowned, UAB administered group of experts who focus on understanding and treating invasive fungal infections and have led most of the clinical trials for FDA-approved antifungal treatments. (Mycology is the study of fungi; mycoses are invasive fungal infections.)
Why do fungi love Alabama? Geography is one big reason. “We are in the hot, humid Deep South, and our soil and flora contribute as well,” Pappas said. This is not necessarily a bad thing. “If fungi weren’t here, the Earth would be covered with plants and trees and organisms that had never decayed,” Pappas said. “Their primary purpose is to break down organic material into its elementary components. Sadly, they can do the same thing to people.” And unfortunately, “our population in Alabama tends to be sicker” and immunocompromised, Pappas said. “We have a large group of transplant recipients, HIV patients, and people on immunomodulation therapy for diseases such as lupus. The environment in Alabama is like the perfect storm.”
A spreading storm
But Alabama’s bad news is also good news in a world where fungi are becoming a global health threat. Most fungi cannot survive the 98.6-degree temperature of the human body, but a warming planet is changing that. And widespread use of industrial antifungals—sprayed on crops and mixed in with paint, among many other applications—is increasing resistance to the limited number of antifungal treatments on the market. Worldwide, fungal diseases kill more than 1.5 million people each year, and the number is rising. Alabama’s climate and population, and UAB’s reputation, mean that patients here benefit from the expertise of specialists such as Pappas and Sixto Leal Jr., M.D., Ph.D., director of the Division of Laboratory Medicine in the Department of Pathology, whose hospital labs can track the spread of fungal infections like nothing else in the region. That gives Alabama an advantage as new fungi are on the march around the world.
The HBO hit series “The Last of Us,” and the video game that inspired it, revolve around a fictional fungus-based apocalypse. Meanwhile, reality has contributed its own fungal supervillain: Candida auris. This treatment-resistant yeast, with a mortality rate of 60 percent, was first identified in 2009 in Japan and appeared in the United States in 2013. More than 2,377 people in the U.S. were infected with C. auris in 2022, according to the Centers for Disease Control and Prevention (CDC)—up from 53 in 2016.
“Most yeasts like to be in a moist environment—wet soil, pigeon droppings, the GI tract,” said Leal, who is director of ground zero for C. auris testing in the UAB Health System: the Clinical Microbiology Lab for UAB Hospitals and the UAB Fungal Reference Lab. “They live within you, so you don’t have to worry about getting it from a door handle or sheets,” Leal said. “But C. auris can live outside the body, so it spreads. It can hang out in rooms and live on bedsheets.”
Alabama did not have a C. auris case until 2022, when it was identified by Leal’s lab. Since then, five more Alabama cases have been reported to the CDC’s database. So far, “all the patients with C. auris at UAB have been susceptible to micafungin, the first-line therapy for anyone in the ICU that you think may have fungus in the blood,” Leal said.

Left to right: Peter Pappas, M.D. and Sixto Leal, M.D., Ph.D.
Renowned Experts
Leal’s labs, perhaps the best equipped in the state, can rapidly identify C. auris and thousands of other pathogens using two state-of-the-art MALDI-TOF machines. One is “the size of a Coke machine” and the other is a bit smaller. The test itself is high-tech, fast, and cheap. “You start with a little slide that resembles an old Scantron bubble sheet,” Leal explained. “Instead of a No. 2 pencil, you fill in each bubble with a toothpick touched to a [fungal] colony on an agar petri dish.” Inside the machine, “a laser zaps the organism and ionized protein fragments travel through a vacuum and strike a detector recording a spectrum that is unique for each species,” Leal said. “With MALDI, you can fill in that bubble in 10 seconds and it costs about 75 cents to get a result. It is way cheaper, faster, and more accurate than biochemical panels, enabling us to rapidly identify thousands of fungi, molds, and bacteria.”
“Since Sixto joined us [in 2018], it has allowed us to explore things in much more detail,” Pappas said. “We are able to do more rapid molecular-based diagnostics, which let you distinguish different strains of organisms. That allows us to explore and understand and deepen our fungal enterprise. He is pushing the envelope with respect to diagnostics that are more aggressive and emerging.”
Leal and Pappas have national reputations in their fields. When the magazine of the College of American Pathologists ran a major feature on how hospital labs were handling C. auris infections, it put Leal on the cover and quoted him extensively throughout. When the Wall Street Journal published a series of reports on C. auris and the fungal resistance to drugs, Pappas was quoted at the top of each article.
Another comment in one of those Wall Street Journal stories, from Tom Chiller, M.D., leader of the CDC’s Mycotic Diseases Branch, captures the urgency experts feel at the moment. “We desperately need new drugs,” Chiller said.
Pappas and Leal each have received major research awards recently for their fungal research. In September 2023, the Mycoses Study Group was awarded a five-year, $7.5 million U01 grant from the CDC, with Pappas as principal investigator. The grant is funding extensive studies on the use of industrial antifungals and antifungal resistance nationwide.
Leal, who is the scientific director of UAB’s regional biocontainment facility, also has an active research program. In 2022, he received a four-year, $2.97 million R01 grant from the National Institute of Allergy and Infectious Diseases to study the underlying mechanisms of COVID-associated fungal infections. “Approximately 5 to 10 percent of individuals with severe COVID develop secondary mold infections, including COVID-associated pulmonary aspergillosis, or CAPA,” Leal said. “We are trying to understand how viral infection makes otherwise healthy individuals vulnerable to mold infection.”
Testing New Therapies
Thanks to UAB’s position in the Mycoses Study Group and Pappas’ reputation in the field, UAB investigators are helping to test most of the new antifungal drugs in development. Pappas was part of a group of investigators who published results from a Phase 2 study of one promising new treatment from Pfizer, Fosmanogepix, in May 2023.
Fosmanogepix is part of “a new class of drugs,” Pappas said. “Most antifungals work at either the cell wall, which is on the outside, or the plasma membrane right on the inside. Fosmanogepix interacts with anchor proteins that are directly involved in plasma membrane and cell wall synthesis. The important thing is that it is a different mechanism of action. There are relatively few drugs and few mechanisms of action for treating fungal diseases. Doctors have only a few choices, and that is one of the things that make fungi difficult to treat. The drugs you can use that are not super toxic are pretty limited.”
The benefit of having a new class of drugs, “is it allows you to perhaps treat different fungi or treat certain fungi better,” Pappas said. “For instance, Fosmanogepix hits C. auris really hard. But there is another Candida species that it doesn’t hit at all.”
Pappas and UAB also are involved in trials for an oral drug called Ibrexafungerp. The drug was approved by the Food and Drug Administration in 2021 to treat vaginal yeast infections, and experts want to know whether it can treat more severe diseases.
The UAB team also is involved in studying a next-generation drug called rezafungin, given weekly as treatment or prevention of fungal infection in selected patients. The ReSTORE Phase 3 trial, published in The Lancet in January 2023 with Pappas as senior author, studied efficacy and safety outcomes of a weekly dose of rezafungin in patients with candidemia and invasive candidiasis, demonstrating similar efficacy to standard-of-care treatment for this condition.
Todd McCarty, M.D., associate professor in the Division of Infectious Diseases, is the principal investigator for the ReSPECT trial at UAB. The ReSPECT study evaluates once-weekly prophylactic treatment with rezafungin compared to daily standard of care for prevention of invasive fungal infections among high-risk patients receiving stem cell transplantation. If it works, this could eventually become the standard of care for high-risk patients, Pappas said. Pappas said he hopes to convince younger faculty members to focus on fungal research—despite a higher profile in recent years, fungi still lag behind viruses and bacteria in research attention, Pappas said.
Why Fungi?
So how did Pappas get into the fungus game? He attended medical school at UAB and returned after stints in Washington, Colorado, and North Carolina. “One of the people who hired me, Bill Dismukes, had a real interest in fungal infection. He steered me in that direction.” (William Dismukes, M.D., was the original principal investigator of the Mycoses Study Group, “and quite a figure in clinical mycology,” Pappas said.) “There was so much of it [fungal disease] here and no one else was doing it, so I tried to fill the vacuum.”
Leal first became attracted to fungi because of the “unique host-pathogen battle—they try to kill you and you try to kill them,” he said. During his M.D./Ph.D. training, “people around the world were losing their eyes,” due to a contact-lens-related global outbreak of antifungal-resistant mold infections, he said. Upon digging deeper, Leal realized that cornea mold infections were a huge global health issue causing blindness in more than 1.5 million people worldwide every year, particularly in neglected tropical communities in India, China, and Africa. Leal established the first mouse model of this disease and worked in Tamil Nadu, India, to evaluate affected patients and the host immune response.
“This experience brought me into medical mycology, and the field has fascinated me ever since,” he said.
- Matt Windsor
As chair of the UAB Department of Psychiatry and Behavioral Neurobiology, Adrienne Lahti, M.D., has a unique perspective on the mental health care landscape in Alabama. “Alabama ranks very low in mental health care,” she said. “In metrics comparing different states’ mental health statistics and access to care, Alabama is usually at 47, 48, 49. The demand is huge.”
Across Alabama, the need for mental health services is often compounded by rural isolation and lack of resources. The Department of Psychiatry and Behavioral Neurobiology is dedicated to bridging that gap, offering a range of innovative programs designed to address the unique challenges faced by the state’s underserved populations. According to Lahti, “The strength of UAB Psychiatry is that it's not only a clinical department, but also one-third of the faculty are researchers, which brings new concepts, new treatments, and new ideas.”
With a compassionate team of experts, cutting-edge research, and a commitment to community, UAB is working to ensure that every individual has access to the support and treatment they deserve. In the following pages, we highlight a few of the department’s programs as well as the providers who are committed to finding innovative ways to get people the treatment they need when they need it the most.

Left to right: Kristine Lokken, Ph.D., and Christina Pierpaoli Parker, Ph.D.,
of the UAB Department of Psychiatry and Behavioral Neurobiology.
Meeting Patients Where They Are
Talk to Christina Pierpaoli Parker, Ph.D., for any length of time and you are struck by her enthusiasm, both for her work as an assistant professor in the Department of Psychiatry and Behavioral Neurobiology and for the growing success of the Integrated Behavioral Medicine Service (iBeMs), the program she proposed and established during her internship in 2020. The service is designed to work directly with primary care physicians to improve referral and follow-through rates of primary care patients in need of behavioral and mental health treatment.
“Primary care has been the de facto mental health system since the 1970s in the United States,” said Parker, who is the program’s director. “Most people with psychological symptoms don’t have access to a psychologist or psychiatrist, or they may have a negative view of mental health care. So, they go see their primary care physician instead. But for many reasons, those patients do not get referred, or if they do, they do not follow through. That’s why integrating behavioral health into the primary care setting just makes sense, because that’s where it’s happening.”
Or more precisely, where it’s not happening. According to data, without a service like iBeMs, primary care physicians recognize less than 50 percent of their patients needing behavioral or mental health care and just 15 percent of those recognized make it through a referral.
When Parker approached her department leadership about starting iBeMs, she found a receptive audience in Kristine Lokken, Ph.D., chief psychologist and professor, and Rachel Fargason, M.D., Patrick Linton Professor, senior associate director of Strategic Planning, and Medical Quality Officer. “Dr. Fargason has always been a champion of integrated medicine but UAB had a few starts and stops with it,” Lokken said. “She was excited to have someone lead the charge.”
Parker put iBeMs into service, embedding it first within two clinics: UAB Medicine Primary and Specialty Care of Gardendale and UAB Nephrology at the Kirklin Clinic. It most recently expanded to the UAB Camellia Medical Group.
During the week, Parker and her associates, a doctoral student and an intern, travel from clinic to clinic consulting with physicians and helping them to identify patients who need care. If behavioral health care is needed, an appointment will be set to see the patient in the familiar environment of their physician’s office. In cases of more immediate symptoms, such as a panic attack or suicidal ideation, an iBeMs team member will travel to the office to see the patient while he or she is there, conduct an assessment, and plan a course of action. If the assessment concludes that medication is advisable, a referral can be made to a psychiatrist. In all cases, the physician receives a comprehensive report on findings and actions to be taken.
The numbers racked up by iBeMs tell a story of success. Data show that when referrals to psychological care are made from primary care, there’s a 75 percent chance that the patient does not follow through. However, with integrated care referrals, the follow-through rate skyrockets to 90 percent.
“We’ve seen that here with Christina,” Lokken said. “In addition to her iBeMs ‘baby,’ she has two actual babies, and while she was on maternity leave, we had a really high no-show rate that recovered when she returned.”
Integrated behavioral care, said Lokken, benefits all areas of care. It gives physicians the confidence to address patients’ issues and reduces provider burnout by referring patients to the appropriate care. It helps patients with their psychological issues and helps them take control of health issues, reducing the patient load for providers. Downstream, integrated care helps reduce emergency department visits by people mistaking psychological issues for physical issues, such as mistaking panic for a heart attack.
With characteristic enthusiasm, Parker shares her vision for iBeMs’ future. “My ultimate goal is to have behavioral medicine integrated into every nook and cranny of the health system, regardless of the clinic. So, if you are struggling with cancer, I want you to be able to see a behavioral health specialist there. If you’re struggling with incontinence, I want you to see a behavioral specialist there. If you are struggling with COPD, with dialysis, with gynecological issues, I want you to be able to see a specialist in each of those clinics.”

Left to right: Leah Pickett, DNP, CRNP, and Rachel Fargason, M.D., lead the UAB Esketamine Clinic.
Esketamine Clinic Transforms Lives
“Serendipity” isn’t a word one might associate with treatment resistant depression (TRD), a type of depression that defies traditional medication. But when describing the development of esketamine as an effective treatment for the disorder, serendipity plays a key role.
“Esketamine is a form of ketamine, a drug that was first used as a sedating or anesthetic agent in horses,” Fargason said. “Ketamine has also been used for decades as a brief surgical anesthetic in human patients. It’s here that we serendipitously discovered its effectiveness in treating TRD.”
Psychiatric patients who struggled with TRD and who had undergone surgery frequently reported feeling much better, Fargason said. Better yet, she added, those with suicidality reported feeling better right away, as opposed to the weeks it can take for other medications to take effect.
Soon, the buzz around ketamine and its effects on TRD triggered a series of international clinical trials. UAB participated in several trials on the S(+)chemical isomer, the stronger of ketamine’s two enantiomers, hence the “esketamine” moniker. Unlike racemic ketamine, which must be given intravenously, this agent can be given intranasally. It wasn’t long before a new word was bandied about: breakthrough.
In 2013, the U.S. Food and Drug Administration (FDA) granted esketamine a “Breakthrough Therapy Designation” to accelerate studies of its effects on TRD, the first antidepressant to receive this designation. Those studies led to the development of the esketamine nasal spray Spravato™, and none too soon.
According to a 2021 study, an estimated 8.9 million Americans experience and are treated for major depressive disorder (MDD). Despite trying multiple traditional antidepressants, 2.9 million of those patients see little improvement and their depression persists.
Esketamine received FDA approval for use in TRD with an accompanying oral antidepressant in 2019, and is FDA approved for use in major depressive disorder with suicide ideation because of its almost immediate effect on suicidality.
“My experience with esketamine is that it opens up a new world of treatment options,” said Fargason, who co-directs the UAB Esketamine Clinic. “The new-age opportunities offered by this agent remind me of when I was a resident and we basically were confined to using the side-effect-ridden tricyclic antidepressants for depression, and then fluoxetine [Prozac] was launched in the U.S. Now, we again have a brand-new medication for patients who’ve been frustrated with years of failed treatment—patients are getting better, getting their lives back, able to work again, able to go back to school, and once again able to participate in and enjoy their family life.”
Esketamine is unique in its mechanism as a non-competitive N-methyl D-aspartate (NMDA) receptor antagonist. Although its mechanism of action is not completely understood, what is known is that the S-molecule increases brain activity of the neurotransmitter glutamate. This increased activity of glutamate increases neuroplasticity—flexibility—of the brain. More flexibility, it seems, enables the brain to manage stress better and helps reverse depression changes.
“It’s really exciting to have this treatment available,” said Leah Pickett, DNP, CRNP, Wellness Manager for Advanced Practice Providers and Esketamine Clinic co-director. Pickett and Fargason worked on the original study that led to the development of Spravato and have served as co-directors of the clinic since its opening in 2020. “We’ve helped a lot of people and that’s very gratifying.”
The UAB Esketamine Clinic recently moved into a larger space, making it more comfortable for patients who must stay for two hours following their dosing. To qualify, a patient must have completed at least two courses of traditional antidepressants, be currently taking an antidepressant they haven’t previously tried, and be referred by their provider.
“A few of our patients have seen effects almost immediately,” Fargason said. “They will come in with a sad or expressionless face and flat affect, and when the treatment is over they are smiling and upbeat. We are able to get most of our patients into remission. About half are able to stop the treatment after the three-month protocol is complete. The other half must come in for maintenance dosing to maintain their remission.
“Often, what we see, though, is that their depression gradually lifts, beyond what a previous medication has been able to do. And that’s what is so exciting—to have a new option to offer. It’s really a joy when you see a patient who’s been so frustrated from years of so many failed trials—sometimes up to 14 failed trials. And here we find that the NMDA antagonist mechanism seems to be the one needed to normalize mood and cognitive functioning to get them back to baseline and being their best self. It’s really exciting.”
Exciting … and serendipitous.
Philanthropy Bolsters Innovation
Depression is the most widespread mood disorder and is often accompanied by shame, guilt, and isolation. In 2022, over 49,000 people in the United States (including over 800 in Alabama) died by suicide, and approximately two-thirds of all suicides are linked to depression.
In Alabama, the burden of depression is particularly heavy. An estimated 157,000 individuals in Jefferson County alone battle depression. The UAB Department of Psychiatry and Behavioral Neurobiology receives a staggering 200 requests for treatment daily.
The UAB Depression and Suicide Center set an ambitious goal in 2017 of raising $10 million to support its mission to increase understanding of and improve treatment for mood disorders. By 2023, this goal was not only met but surpassed, with $10.8 million raised.
As the center’s clinical director, Matthew Macaluso, D.O., has worked collaboratively with other leaders in the Department of Psychiatry and Behavioral Neurobiology to develop clinical programs offering advanced treatments for the most severe forms of depression. These novel clinical programs are directly translated from research conducted by Macaluso and Richard Shelton, M.D., the Charles B. Ireland Professor and center co-director, in collaboration with industry leaders to develop novel mechanism-of-action drugs and devices for severe mood disorders.
The center uses a biopsychosocial patient care approach, crafting personalized treatment plans that can include psychotherapy, intranasal esketamine, vagus nerve stimulation, intravenous ketamine, electroconvulsive therapy, and access to clinical trials of novel therapies. The center will soon add a state-of-the-art repetitive magnetic stimulation treatment device with the MagVenture Atlas Neuro Navigation System. With this addition, UAB will have a cutting-edge program for patients battling depression that rivals what is available anywhere in the world.

Left to right: Richard Shelton, M.D., and Matthew Macaluso, D.O.,
are leaders in the UAB Depression and Suicide Center.
Rev. Gates Shaw, a retired Episcopal pastor, has been a leader in organizing philanthropic support of the center’s fundraising initiative since the center’s inception. “Richard Shelton asked me if I’d chair an advisory board,” Shaw said. ”As I got involved and watched the center gain traction and begin to deliver on its clinical mission, I began to reach out to individuals, foundations, and corporations.”
According to Shaw, while the response he received was mainly positive, he did have to educate some potential supporters. “As with addiction, we sometimes think of depression as a lack of will or a character failure. It's stigmatized, like so many other things, as a personal failure rather than a disease.”
Shaw is quick to share that he has battled depression most of his life and that, as someone who counsels and speaks with people from all walks of life, he is often approached for advice by friends and acquaintances. “I'll be speaking to the board of a foundation and subsequent to that, I'll get a call from one of the board members saying, ‘I'd like to talk to you about my son,’ or ‘I'd like to talk to you about my wife,’ or ‘Can you can you help me understand what is going on?’ So, depression sits right beneath the surface in so many families. And speaking with authority about it means I have to say I know what it is to suffer from depression, and I know what it is to get well,” Shaw said.
Thanks to the outstanding success of the fundraising initiative, as well as a series of impressive grant awards, the center is growing, both in size and impact. “We now have 20 faculty members and literally dozens of research staff and trainees,” Shelton said. “We have delivered a more than five-fold return on investment so far. Since its inception, our center has received more than $55,000,000 in federal grants, industry contracts, and foundation support. Our research programs and clinics will continue to expand into the future.”
A new, $6 million fundraising initiative in the department, the Early Intervention Program, aims to step in early in the course of mental illness, thereby improving the chances of treatment success. “When you look at the onset of mental illness—depression, schizophrenia, substance use disorder—it is in late adolescence/early adulthood,” Lahti said. “So we want to address it at the onset, or as close to the onset as possible. We know that the longer you wait to treat the worse the outcome. In addition to being the chair, I do research on brain imaging and you can see that the longer you wait to treat people, the worse the communication between brain regions, so the brain is losing plasticity.”
The Early Intervention Program fundraising initiative is already over halfway toward its goal, and Lahti is optimistic the goal can be met to get the program off the ground. “I'm totally amazed by the generosity of the community toward our Department of Psychiatry,” she said. “ Their support is incredible. I've never seen that before at other places.”
While the Depression and Suicide Center’s fundraising goal may have been met, Shaw continues to champion the department’s work and the new early intervention initiative. “Ultimately, I want to see people walking around cured. Fortunately, that is also in the heart of the chair of the department, Dr. Lahti, and the center leadership—they, too, want to see people cured.”

As our society evolves so, too, do the health challenges we face.
UAB Medicine is at the forefront of addressing emerging and evolving health issues with the introduction of new clinics and programs designed to meet the dynamic needs of patients at every stage of life. Among these are the UAB Comprehensive Smell and Taste Clinic, which responds to the increased prevalence of smell and taste disorders following the COVID-19 pandemic, providing specialized care and innovative treatment options. The UAB Staging Transition for Every Patient (STEP) Program ensures that adolescents transitioning from pediatric to adult health care receive seamless, comprehensive care, bridging a crucial gap in patient management. Additionally, the UAB Brain Aging and Memory Hub offers holistic services for those experiencing cognitive decline, integrating advanced research and personalized care to support individuals and families navigating the complexities of aging and memory loss. These initiatives underscore UAB Medicine's commitment to pioneering solutions for contemporary health challenges, ensuring patients receive the highest quality of care tailored to their specific needs.
Do-Yeon Cho, M.D., (left) and Carly Bramel, P.A., (right) run the UAB Comprehensive Smell and Taste Clinic.
Passing the smell test
Since the beginning of the COVID-19 pandemic, at least 500,000 Alabamians have experienced extended smell and taste loss, according to Do-Yeon Cho, M.D., director of the UAB Comprehensive Smell and Taste Clinic and a professor in the Department of Otolaryngology. The clinic, which opened in January 2023 and is thought to be the first specialized clinic in Alabama for patients with olfactory dysfunction, has seen a high volume of patients, with appointments booked far in advance. Luckily, the outlook for most patients is ultimately positive. “After two years, about 80 to 90 percent recover,” Cho said.
COVID and the media attention around COVID smell loss have brought more people to clinics such as Cho’s, but that does not mean every patient’s smell loss can be attributed to COVID, even if a COVID infection was the first time they noticed it.
“I examine patients every time they come in,” Cho said. “A lot of patients did indeed lose their sense of smell from COVID, but some have foreign bodies in their noses, and others have large nasal polyps.” These polyps are often the result of allergies. “We have a lot of pollen in Alabama,” Cho said. “Inflammation or nasal polyps can both block the nose and alter the sense of smell.” Treatment in this case is a steroid rinse.
Cho also asks patients about other symptoms. If they have headache or another neurogenic issue, he will often recommend an MRI or CT imaging scan of the brain and, if warranted, a referral to a neurologist. Cho will also talk with patients or caregivers about their family history of Parkinson’s disease or early-onset dementia. “Smell loss can be the first symptom of neurodegenerative disease,” Cho said. If the cause is related to neurodegenerative disease, “Patients will often say they have noticed it for a few years.”
After a physical exam of the nose and a discussion of symptoms and timing, Cho uses threshold discrimination identification (TDI) testing to evaluate the severity of smell loss or dysfunction. “We are probably the only location doing TDI testing in Alabama,” Cho said, calling it the gold standard for testing. Patients smell a series of odors from what look like felt-tip pens. The odors are at various concentrations—the testing gives an objective score measuring the patient’s ability to distinguish smells from one another and to distinguish the intensity of smells.
While researchers continue to debate the underlying reason for smell loss or dysfunction, smell training is helpful for many patients. “Thirty to 40 percent of patients see significant improvement” after smell training, Cho explained. The training helps rebuild the connections between the nose and the brain and helps patients relearn to accurately identify types of smells.
Cho said smell training kits can be assembled using products that are readily available in stores or online. “You can absolutely use essential oils,” he said. “We recommend four smells at a minimum, although more is great.” The recommended categories of smell include a fruity, sweet smell (like lemon), a flowery smell (rose), a spicy smell (clove), and a resinous smell (eucalyptus).
Cho recommends that patients “get in a zen place” of mental calm. They should hold the tube under the nose for 30 seconds and breathe normally, concentrating on the scent before moving on to the others. “Think about the smell, even if you can’t smell that well,” or at all, at first. “Once you can smell it well, move the tube farther away.”
A subset of patients with olfactory dysfunction do not lose their sense of smell. Instead, it is altered, usually for the worse. “Everything smells terrible,” Cho said. For patients suffering from parosmia, smells can be so off-putting that many “are not able to eat or drink, and there can be severe weight loss,” Cho said. “One patient described taking seven showers a day, trying to get rid of the smell.”
The biological cause of parosmia needs more study, but it comes down to “an issue of how certain odors are interpreted in the brain,” Cho said. “We think this may happen when smell nerves are recovering and they go to the wrong parts of the brain and become overactive, firing too much.”
Cho recommends smell training for these patients, but he has also used the anti-seizure medicine gabapentin with significant success. In 2022, Cho published a paper about a small clinical trial in his clinic.Over the course of the trial, gabapentin was prescribed to 12 patients.
Of the nine patients who completed the study, eight showed improvement and six patients (66 percent), all of whom had parosmia with a foul smell, reported significant improvements. “They did really well,” Cho said. “It shows that, in certain people, medications can help.”
– Matt Windsor

(Left to right) Carlie Stein Somerville, M.D., Betsy Hopson, and Snehal Khatri, M.D., help patients with complex diseases of childhood transition to adult care through the UAB Staging Transition for Every Patient (STEP) clinic.
Living Longer, Healthier Lives
“In the first years of my practice, I saw there was a gap for patients between 18 and 21 years old who had complex diseases of childhood like spina bifida or cerebral palsy, which can have a lot of medical and caregiver needs as they grow up,” said Carlie Stein Somerville, M.D.,an associate professor in the Division of General Internal Medicine. “I wanted to help doctors understand how to help these patients and their families. We are so fortunate to have crosswalks from Children’s of Alabama to the ‘adult hospital’ at UAB. I wanted to create a similarly streamlined transition care from one hospital to the other for our most complex patients.”
In partnership with Betsy Hopson, then the program director for the UAB and Children’s of Alabama Spina Bifida Program, Somerville launched the UAB Staging Transition for Every Patient, or STEP, Program, to help patients across the health system make the leap.
“There is a gap when patients transition from pediatric to adult clinics,” Hopson said. “Life changes are happening—they are leaving high school, trying to figure out what comes next, and right in the middle of that you have this transition in medical care, with brand-new doctors. If you look at the data, you see how medical outcomes decline during this time.”
The nationally recognized STEP Program was funded by a grant from UAB’s unique Health Services Foundation General Endowment Fund grants program. “This is an outpatient primary care clinic where patients and their caregivers can meet a multidisciplinary team to work through the pieces of transition,” Somerville said. “The clinic has three med-peds-trained physicians and seven specialists who come to the clinic and see patients.” These include specialists in psychiatry, psychology, pulmonary, endocrinology, neurology, epilepsy, rehabilitation medicine, physical therapy, and social work.
Gathering all these specialists in a single clinic, who can see patients during a single clinic visit, “helps with navigating Birmingham and parking decks and traveling with all the equipment that these patients often require,” Somerville said. “They get coordinated care and connect to all the adult subspecialists they need.
“There are no other programs like this in the region and only a handful in the country,” Somerville said. “Now we are up to 600 patients, and we are seeing patients from all over the state who travel to us to get this level of care.”
The providers have also benefited. “Any doctor who needs help transitioning a complex patient” can work with the STEP clinic, Somerville said. “As someone who has been a primary care doctor myself, my goal is to empower others to be comfortable taking care of these patient populations, to know about STEP and what we offer, and that they can call us.”
Thanks to its success, the STEP Program has spun off a program aimed at the particular needs of a subset of patients. As recently as the early 1980s, people with Down syndrome were not expected to live past 25. Today that number is up to 60 years old. But longer lives come with questions that few doctors or parents know how to answer.
For instance, many of the relatively small number of people with Down syndrome who have lived to age 40 have developed dementia and other Alzheimer’s-like symptoms by then. But the medications doctors use to treat Alzheimer’s are not approved for people this young.
“We hear from parents that this is the thing they worry about the most,” said Snehal Khatri, M.D., associate professor in the Division of Developmental and Behavioral Pediatrics, and medical director of UAB Sparks Pediatrics. With a grant from UAB’s HSF-GEF program, Khatri and Hopson, STEP Program director, are creating a new clinic within the STEP program to focus on care for people with Down syndrome across the lifespan. It is a very different experience in the pediatric world and the adult world ... Insurance changes. What is covered changes. So being thoughtful in planning for these changes early is extremely important.”
The American Academy of Pediatrics and the Down Syndrome Medical Interest Group publish guidelines from birth to age 21, including lab work, questions to ask, and other milestones to look for as patients age. But “you would be surprised at the number of primary care doctors who don’t know they exist,” Khatri said. “Having a dedicated clinic will improve adherence to medical guidelines for the pediatric patients.”
The link between pediatric and adult services also means that good ideas can be quickly shared. “One of the things that has been successful at Children’s of Alabama is recognizing sensory needs and the development of sensory pathways” for patients with autism, Down syndrome, and other intellectual disabilities, Hopson said. “What STEP has allowed us to do is to put teams and working groups together to determine what successful practices from pediatric care should or could be brought into the adult clinics. When you think about it in terms of lifespan, what makes it work well from 0–18? Why was the family so comfortable? Let’s adopt those practices with the adult patients. And we are also learning from our adult providers when they say things like, ‘I see patients who are 21 and don’t know they can get pregnant.’ That calls for education on the pediatric side. There is a two-way education stream.”
The lifespan model has potential beyond Down syndrome, Khatri points out. “There are so many conditions that we see in pediatrics that don’t have a good home: autism, dual diagnoses. Is this a framework for other conditions that also cross over from the pediatric to the adult world? We aim to find out.”
- By Matt Windsor
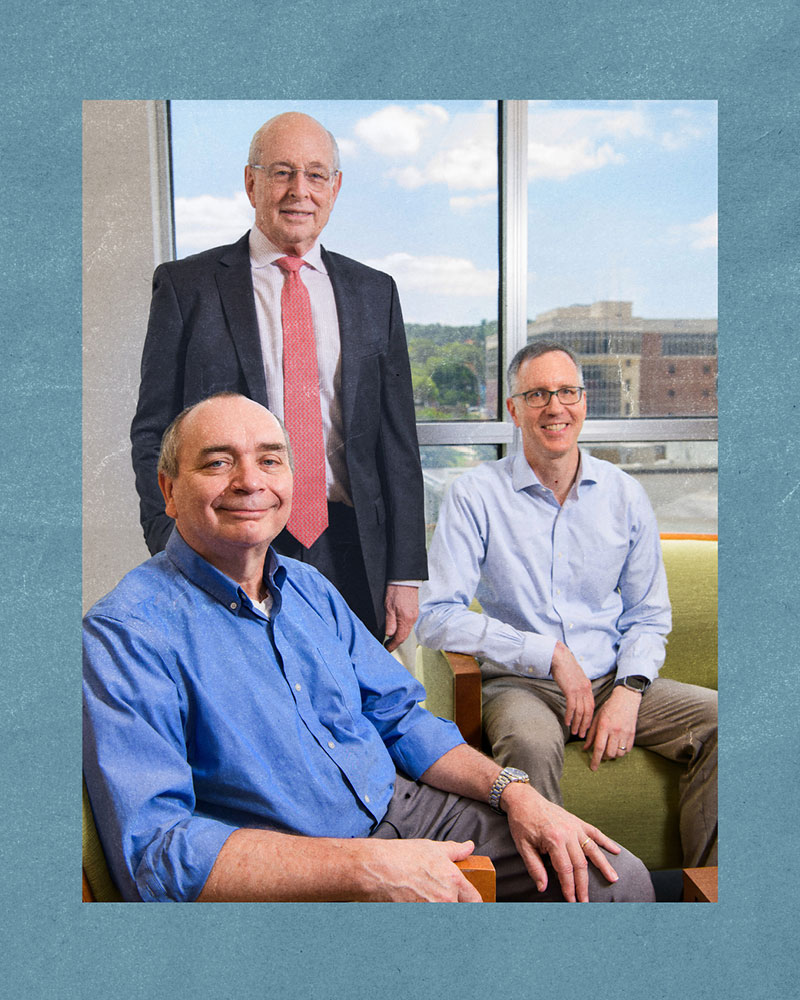
(Clockwise from top) Ronald Lazar, Ph.D., Erik Roberson, M.D., Ph.D., and David Geldmacher, M.D., are now providing care and conducting research from the new Brain Aging and Memory Hub at UAB.
Memory Matters
In April 2024, UAB celebrated the opening of the UAB Brain Aging and Memory Hub, a joint effort between the UAB Health System and the Heersink School of Medicine. The nearly 20,000-square-foot Brain Aging and Memory Hub is located on the newly renovated fifth floor of UAB Callahan Eye Hospital.
Today as many as 80,000 Alabamians have possible early signs of memory problems. Additionally, Alzheimer’s disease is ranked second in Alabama’s state mortality rate. The new hub was created to anticipate the increasing needs of an aging population and will address the full spectrum of cognitive brain health and memory disorders.
The hub houses two divisions in the UAB Department of Neurology: the Division of Neuropsychology and the Division of Cognitive and Behavioral Neurology. In addition to the two divisions, the Alzheimer’s Disease Center and the UAB Evelyn F. McKnight Brain Institute are located in the new space.
“We were tasked with a mission to create a new care model that would advance the research and meet the clinical needs of our patients,” said David Geldmacher, M.D., director of the UAB Division of Cognitive and Behavioral Neurology. “We realized we did not need more of what we’ve been doing, but rather needed to develop a different system altogether. The new hub is a unique, integrated model that we have yet to see at other institutions.”
Memory disorders are often complex conditions and require a team approach, including neurologists, nurses and nurse practitioners, nurse care managers, pharmacy specialists, and social workers and counselors. The new Brain Aging and Memory Hub will increase collaboration and streamline efforts from prevention to research to clinical care.
“Each member of our team plays a crucial role in fostering research and compassionate care for our patients,” Geldmacher said. “Being able to walk down the hallway, instead of hopping on a call, will eliminate barriers and create a more cohesive and effective environment.”
Ronald Lazar, Ph.D., director of the Division of Neuropsychology and UAB Evelyn F. McKnight Brain Institute, and his team look forward to advancing brain aging and cognitive decline research and care in the new hub. “Studies show that 40 percent of all dementia cases can be either postponed or prevented entirely,” Lazar said. “There are lifestyle behaviors and risk factor management tools that can mitigate and prevent future memory problems. We want to promote brain health across people’s lifespans, not only once they hit 60.”
In May 2024, the UAB Alzheimer’s Disease Research Center (ADRC) received a $21.4 million award over five years from the National Institutes of Health. This is a significant advance toward addressing the disproportionately high rates of Alzheimer’s disease and related dementias in Alabama and the Deep South. Contributing to this disparity, the region is populated with groups disparately impacted by dementia due to factors associated with race, adverse social determinants of health, chronic health conditions, and other issues. The region is also home to the nation’s largest population identifying as Black or African American, who are estimated to be at double the risk of Alzheimer’s disease.
Realizing the center’s vision of a future in which these disparities in Alzheimer’s disease are eliminated requires a deeper understanding of how this unique amalgamation of factors drives higher rates of dementia. Previous funding from the NIH’s National Institute of Aging has helped the center establish the teams, programs, and infrastructure to pursue this goal, and it has exceeded recruitment goals with a cohort that is nearly 60 percent Black/African American.
With the new funding, the ADRC, led by Erik Roberson, M.D., Ph.D., will build on this initial track record of success by providing coordinated infrastructure that leverages UAB’s strengths to answer questions necessary to reduce Deep South disparities in dementia. It will also continue recruiting a cohort that reflects the unique and diverse population of the Deep South and collecting a broad dataset from participants that informs about potential foundations for Deep South disparities in Alzheimer’s disease and related dementias (ADRD), including clinical, social determinants of health, activity/sleep, genetic, and biomarker data. By collecting and sharing biospecimens from participants in a unique Deep South cohort with researchers across the country, the ADRC will help increase diversity in national ADRD initiatives; foster innovative and impactful ADRD research, especially projects addressing Deep South disparities in dementia; attract and train the next generation of ADRD researchers; and increase awareness of ADRD among the public and at UAB.
– Hannah Echols

In the early 1980s, a hit TV show introduced many Americans to artificial intelligence (AI). While Michael Knight, famously portrayed by David Hasselhoff, was technically the main character of “Knight Rider,” it was KITT, a black 1982 Pontiac Trans Am with the power to think and talk, that spurred fans of the show to tune in week after week. Forty years later, AI is causing changes in the medical field that would have read like science fiction not that long ago. In fact, experts at the Heersink School of Medicine do not hesitate to say that AI is in the process of revolutionizing the profession. “It’s hard to imagine an area of medicine that’s not going to be changed by AI,” declared Matt Might, Ph.D., director of the Hugh Kaul Precision Medicine Institute. “It’s going to redefine medicine on every level,” echoed Rubin Pillay, M.D., Ph.D., executive director of the Marnix E. Heersink Institute for Biomedical Innovation and Chief Innovation Officer for the UAB Health System. “It’s changing so fast that it’s hard to say where it’s going, except that it’s going to be everywhere,” said James Cimino, M.D., chair of the Department of Biomedical Informatics and Data Science. So what are the real-world consequences of using artificial intelligence in the medical field? Is Dr. Robot on the horizon? Here we take a look at some of the ways AI already is being used within UAB Medicine, and a glimpse at what may be on the horizon sooner rather than later.
Filling in the Blanks
It is a routine that has been taking place for generations. A patient tells a doctor what is wrong. The doctor asks questions, runs tests, makes a diagnosis, and recommends a treatment plan. If the first approach doesn’t succeed, they try again. Technology has already improved this type of trial-and-error exchange, and AI can improve it further, according to Cimino. He sees signs of how this can work through the use of generative AI like ChatGPT.
“Clinicians approach a patient’s problems starting with what they know and turn to knowledge resources as needed to fill information gaps. We used to build decision support systems that would try to anticipate the need for that information, but development was slow, expensive, and difficult to maintain,” Cimino said. “The emerging generative AI tools draw on an enormous set of information and can synthesize connections on the fly to bring better relevant knowledge to the point of care based on patient-specific data.
“I used to formulate questions about a patient, turn to various knowledge sources like text books, expert systems, or PubMed, and create a query to find what I thought might be relevant to the patient’s case. Now, I can put the patient’s information into something like ChatGPT and ask questions in plain English, let it retrieve relevant information from multiple sources, and integrate it all into a single (usually coherent) response.”
The immediate benefit is not only the ability to store all this medical data but also to distill it down to the most salient information, making it easier for patients and physicians to comprehend and communicate. “We have electronic health records that pull data from many different sources (such as clinicians’ notes, orders, and ancillary reports) into one place, but it is really difficult to navigate,” Cimino said. “If I put that whole record into generative AI and say, ‘Summarize this patient’s record for me,’ it will do it. Then patients can use this resource to help them understand their conditions.
“We also have what are called genomic-informed risk assessments, and they can be 25 pages long. I’m a physician and a researcher and even I have difficulty with them. I’ve taken those and asked ChatGPT to rewrite them for a person with a high-school education, and then again for a person with a sixth-grade education. It was simply amazing what it produced. This has tremendous potential.”
Taking it one step further, Cimino said he can foresee the day when there will always be a readily available second-opinion (and a third and fourth, if needed) in the form of AI. He said such a system could give a physician live advice as the initial patient-analysis process is taking place.
“There are a lot of things generative AI could eventually do if we can bring it to the point-of-care in an unobtrusive way,” Cimino said. “What if the computer can say to the doctor, ‘You should ask the patient this question.’ Physicians might find it annoying at first, sort of like a backseat driver, but once they realize that it can help them quickly diagnose something they might otherwise have missed, I think doctors and patients will appreciate it.
“Then we can give all this information to a generative AI system, and it can analyze it in the context of the patient’s care and say, ‘You need to pay attention to these genetic markers that this patient has.’ That is going to be a tremendous benefit.”
Cimino said these are just some of the many ways that AI technology can benefit medicine and makes physicians’ jobs easier. “It’s hard to imagine a problem we face in medicine that would not be made at least somewhat better with this,” Cimino said. “There are a lot of creative ways we can be using this at every point in the care process. Then along with better care, we have better data for research and discovery.
“Ultimately what we’re always trying to do is improve human health. And this new wave of artificial intelligence can help at every step of the way.”
AI in Medicine Master’s degree
In June 2024, UAB launched a Master of Science degree in Artificial Intelligence in Medicine (AIM), established collaboratively by the Heersink School of Medicine and the Marnix E. Heersink Institute for Biomedical Innovation (MHIBI). The new graduate degree program is the first of its kind in the Southeast and is designed to equip trainees with the specialized technical skills to manage large medical datasets for AI development.
“As part of graduate dissertation research, students will engage in cutting-edge research at UAB, collaborate with faculty experts, and utilize state-of-the-art AI labs across UAB to gain a comprehensive understanding of AI’s practical applications in medicine,” said Sandeep Bodduluri, Ph.D., director
of AI in the MHIBI and the M.S. degree in AIM program director.
The new degree program focuses on the development of sophisticated AI-driven applications for medical imaging and signal processing, as well as the creation of large language models to aid in clinical decision-making. The curriculum—developed in collaboration with the UAB Schools of Engineering, Business, and Health Professions and the College of Arts and Sciences—is structured to provide essential technical training for students who have completed the Graduate Certificate in AI in Medicine.
“At the Heersink School of Medicine and the Heersink Institute for Biomedical Innovation, we recognize the immense responsibility that preeminent academic institutions have in shaping the future of AI in health care,” said Rubin Pillay, M.D., Ph.D., MHIBI director. “Our AI programs are committed to training a diverse group of designers and developers
to create responsible, ethical solutions. We also empower users to make informed decisions about leveraging AI and ensure that individuals, whose data and care are managed by AI, can ask the right questions. Our suite of programming at MHIBI reflects our mission to democratize AI literacy and make
AI accessible and beneficial for all.”
– Alicia Rohan
Curated Biomedical Solutions
In many ways, Matt Might, Ph.D., was AI before AI was cool. He arrived at UAB in 2017 to lead the Hugh Kaul Precision Medicine Institute (PMI), which utilizes computative technologies such as genomic sequencing to personalize disease treatments.
“We’ve been using a form of AI since I got here to identify precision therapeutics,” Might said. “The thing that has changed is our ability to do it got a lot better very quickly. We’ve been helping patients for years by using this, but sometimes we’d hit a wall and we couldn’t go any further.
“Now we have a whole new way to creatively reason about ways to help patients that we didn’t have access to before. The kind of creative reasoning that AI can do to help patients is really remarkable. That’s one of the things that’s so powerful about this.”
As a recent example, Might said the PMI received an emergency outreach from the UAB Division of Infectious Diseases regarding a patient suffering from an extremely rare pathogen who was not responding to the only known treatment. Might’s team gathered all the available information, then began using AI systems to run case reviews in search of possible alternatives for care. The results surprised even Might.

From left to right: James Cimino, M.D., Matt Might, Ph.D.,
and Rubin Pillay, M.D., Ph.D.
“Within about an hour, we had five or six potential ideas—with scientific justification—for why these treatments might help this patient,” Might said. “We couldn’t have done that even a year ago. We just didn’t have the ability to deploy creative reasoning that quickly to come up with powerfully curated biomedical solutions.
“For us, a lot of this is not necessarily new because we’ve been using AI the whole time. But we’re definitely able to do it better now, there’s no question about that. And that has us revisiting precision diagnostics, because these newer generative AIs are really good at creative reasoning around potential diagnoses.”
Moving forward, Might said AI systems are proving to be extremely helpful in PMI’s work as part of the coordinating center for the national, NIH-funded Undiagnosed Diseases Network, which was established in 2014 to provide diagnostic assessments for patients with chronic, undiagnosed medical conditions.“We’re in contact with thousands of undiagnosed patients around the country who are on long diagnostic odysseys,” Might said.
“We’re using AI to summarize all the medical records and start making predictions around their diagnosis.” Humans were doing this previously, but it was an incredibly labor-intensive process, and it really limited how many patients we could help. Our goal now is to use AI to massively increase the scale of the number of patients we can help.”
Similarly, Might said AI will be able to alleviate issues that all physicians currently face in terms of daily administrative tasks that use up valuable time they could be spending trying to help patients. “You could have an AI listening in on a conversation between a physician and a patient, and then create a transcript that can be transformed almost automatically into any number of forms,” Might said. “This includes transforming it into code that can automatically draft any orders the physician mentioned during the consultation.
“Eventually we’re going to have intelligent surveillance of every engagement, every encounter, within the entire health system. I think AI will end up becoming a gigantic safety net around a health system to make sure that a patient doesn’t fall through the cracks.”
Even for a man whose career has long lived on the leading edge of technological advancements, Might said he is amazed at the sudden potential AI is unlocking within the medical field.
“This has been one of the strangest moments of my professional life,” Might said. “In computer science, we knew we would get here at some point. What has surprised even the computer scientists is how fast it has happened. It has emerged far sooner than anyone expected.”
Science Fiction come to life
Mistakes happen. Humans are fallible, after all. But Rubin Pillay, M.D., Ph.D., wants to see the number of mistakes that take place within the medical field drastically reduced. And he says the solution will be to not rely solely on humans.
“If you look at health care delivery globally, our diagnostic and therapeutic error rate is about 12 percent and preventable deaths are around 400,000 cases a year in the U.S. alone,” Pillay said. “It’s a problem that needs to be addressed, and AI and medical automation is going to help us get there, like it has in many other industries. Automation has essentially democratized access to most products and services, and it will do the same in health care.
“We’re not far off from a time where we’ll be questioned if we’re using solely human capacity and capability to deliver care. Probably within the next five years, most physicians will augment themselves with AI, and it’s something that we need to do.”
In fact, Pillay said the medical profession is in the early stages of being entirely transformed by AI. When asked what areas of the field will be affected by this technology, he quickly replies, “Pretty much everything.”
“The immediate impact is on the operations and administrative side, which is a huge burden,” Pillay said. “One of the leading causes of physician burnout is the administrative functions that they perform, and technology is rapidly improving that. It’s going to allow physicians to spend more quality time with patients, which will result in better care and better patient outcomes.
“On the clinical side, we’re still a little bit away from AI having a tangible impact on care delivery.” However, Pillay said that will soon change, and eventually AI will supplement or in some cases replace medical work currently being performed by humans. “There are already AI solutions out there to read radiological images; you upload your image and the AI does the interpretation for you. At the moment, a lot of this is just being used for screening to validate clinical decisions, but we’ve started that process.”
As a result, Pillay said it is crucial for UAB and other medical schools to begin changing the way they train future physicians to accommodate for AI. After all, by the time today’s incoming students complete four years of medical school followed by a residency, it will be the 2030s and many of today’s AI concepts will have become reality.
“The practice of medicine is going to change dramatically, and we’re going to need a revolution in medical training,” Pillay said. “AI is ultimately going to lead to better care delivery, because physicians will be able to use all the available knowledge and data to make clinical decisions, which is humanly impossible to do.
“Eventually the next big leap will be medical automation. There is the potential to replace physicians in certain aspects of care delivery. It’s going to be a leap of faith for both patients and physicians, but it is inevitable.”
After a pause, Pillay added, “It’s science fiction come to life.”
-Cary Estes
Sparking drug discovery
Technological advances such as gene editing, cancer immunotherapy, click chemistry, RNA therapeutics, and cell-based therapy have sparked a growing interest in new approaches to drug discovery. The new Systems Pharmacology Artificial Intelligence Research Center (SPARC)—a partnership between the Heersink School of Medicine and the UAB Center for Clinical and Translational Sciences (CCTS)—is focused on developing new AI-based approaches in disease biology modeling, in silico drug design, and human clinical trials to accelerate drug discoveries while reducing costs. The center is led by Jake Chen, Ph.D., the Triton Endowed Professor of Biomedical Informatics and Data Science.
“Drug discovery has become too costly and too complex for any lab scientist to lead today,” said Chen. “We aim to build critical technology infrastructure fueled by the rapid growth of AI, multi-modality disease biology data, and high-performance computing.”
As a transdisciplinary research center, SPARC will drive innovation in systems biology—the integration of multi-omics data of disease biology—and generative AI to accelerate identification and development of new drugs based on deep understanding of causal human biology and real-world clinical needs.
“The placement of SPARC within our department is timely and appropriate,” said James Cimino, M.D., chair of the Department of the Biomedical Informatics and Data Science. “SPARC researchers will expand the department’s domain of inquiry, while recruitment of new faculty to the department will complement SPARC research by providing a breadth of expertise in areas such as clinical informatics, implementation science, and evaluation.”
“SPARC will build new avenues to cost-effective drug development matched with the emerging AI revolution,” said Chen. “We look forward to building partnerships in an exciting, decentralized drug discovery ecosystem in the years to come.”
– Ryan McCain
The summer of 2024 marked a transformational turning point for health care in Alabama with two important developments. These advances promise to not only improve access to care for people in the Birmingham area and across the state, but also to advance the UAB Health System’s mission to provide life-changing care to all it serves.
As announced June 25, the University of Alabama System Board of Trustees approved an agreement with Ascension for UAB Health System Authority to assume ownership of Ascension St. Vincent’s Health System in central Alabama to sustain patients’ access to the highest quality care in Birmingham and surrounding communities.
Under the agreement, UAB Health System Authority will assume ownership of all Ascension St. Vincent’s sites of care including five hospitals at the Birmingham metropolitan area, as well as the One Nineteen Campus; the Trussville Freestanding Emergency Department; and imaging centers and other clinics that are part of Ascension Medical Group. The transition will include current Ascension St. Vincent’s services, facilities, caregivers, and associates, including a robust network of providers serving the region.
“Patients will continue to have access to the health-care services and providers they’ve come to trust, and ultimately gain access to a larger care network,” said UAB Health System CEO Dawn Bulgarella, who also serves as CEO of the UAB/Ascension St. Vincent’s Alliance. “UAB and St. Vincent’s exist to improve lives, and that purpose will drive our actions in the coming months and beyond.”
The UAB/Ascension St. Vincent’s Alliance launched in 2020 to increase Alabamians’ access to high-quality, innovative medical care and help patients receive the right care at the right time and place. UAB and Ascension St. Vincent’s leadership view this agreement as the natural next step to continue to expand access to sustainable care in Alabama.
Ascension St. Vincent’s CEO and Ascension Senior Vice President Jason Alexander says UAB Health System—with a statewide network of 17 hospitals, both owned and affiliated, and with its integrated care delivery system and proven record of promoting patient-centric, sustainable care across Birmingham and Alabama—is best positioned to extend opportunities for patients to access a larger care network into the future.
“It became clear that adding Ascension St. Vincent’s to UAB Health System’s network of owned hospitals—and combining and optimizing our collective strengths—is the solution to ensure that our community retains access to sustainable, high-quality health care,” Alexander said.
“At UAB Heersink School of Medicine, we are closely aligned with the UAB Health System. By working together, we will be stronger for our patients, our communities, and our employees,” said Anupam Agarwal, M.D., senior vice president for Medicine and dean of the Heersink School of Medicine. “Creating new opportunities for patients to access a larger network of local services will allow us to leverage capacity to better meet patient demand and grow our services. Additionally, this may offer opportunities for more participation in our clinical research.”
At a time when hospitals are closing across the nation, UAB Health System has made it a priority to strengthen Alabama hospitals, support care providers, and increase community outreach and service through innovative partnerships that improve the state’s health-care ecosystem.
“Our mission and vision to provide life-changing care and be the leader in improving the health and lives of all we serve aligns with the outstanding St. Vincent’s caregivers and associates who have served these communities for years,” Bulgarella said. “We look forward to supporting continued operations and providing opportunities for Ascension St. Vincent’s caregivers and associates to essentially remain in their current positions; our goal is to support fulfilling and meaningful careers in service to our patients and communities.”
The transaction is expected to be completed in the fall of 2024, subject to standard regulatory approvals and pending satisfaction of closing conditions and approval by the Catholic Church.
“Since 1898, Ascension St. Vincent’s caregivers and associates have served our community well,” Bulgarella said. “We are excited to honor and continue their culture and legacy, and make sure they feel secure and appreciated in this transition. I look forward to integrating our talented, mission-focused teams as we work together toward continuity and positive results for those we serve.”

Leaders from the Heersink School of Medicine, UAB Health System, University of Alabama Health Services Foundation, and UAB Medical West gathered at the July 11, 2024, ribbon-cutting at the new UAB Medical West hospital campus.
Health care in the greater Birmingham area saw yet more progress when UAB Medical West, an affiliate of UAB Health System, began the transition from its former hospital location—which had been in use since 1964—to a new, $400 million, state-of-the-art replacement hospital with a ribbon-cutting on July 11, 2024.
The new hospital campus, located in West Jefferson County, includes a 412,000-square-foot, nine-story hospital with 200 beds and a 127,000-square-foot, seven-story medical office building. The facility features a new surgical and endoscopy suite, including robotic surgery and 12 operating rooms, state-of-the-art imaging technology, and more intensive care beds. The facility opened to the public in early August, 2024.
UAB Medicine is offering multiple specialty clinics in the new medical office building. Neurosurgery, physical medicine and rehabilitation, cardiology, and pulmonary clinics opened in early August; a rheumatology clinic opened in early September; and an interventional cardiology clinic is scheduled to open in early October. Additional UAB Medicine specialty clinics are expected to open in January 2025.
“To move to our new campus marks a novel chapter for our health-care facility,” said UAB Medical West CEO Keith Pennington. “Our new facility offers West Jefferson County residents and beyond access to unparalleled technology, health care, and services that will meet our patients where they are. We could not be prouder to continue the legacy of Medical West and continue to grow and serve.”
Located less than 30 miles from the Cahaba River National Wildlife Refuge, the new building was designed around nature. Each floor highlights flora native to Alabama, such as the Cahaba lily, azalea, wild hyacinth, honeysuckle, and flowering dogwood. The facility also features a pond with walking trails, rock walls reminiscent of the Cahaba River shoals, floor-to-ceiling windows in patient rooms, rocking chairs, and fireplaces. According to Pennington, “It is a true space of wellness and healing not only for patients, but for our staff members, visitors, and our entire community.”
By Tyler Greer and Alicia Rohan

Each floor at UAB Medical West highlights flora native to Alabama, such as the Cahaba lily, azalea, and flowering dogwood.