Trailblazing Spirit: The journey of passionate hiker and outdoor enthusiast Cindy Louderback

In 2013, Cindy Louderback, an administrative supervisor in the Department of Anesthesiology and Perioperative Medicine, began to embrace her passion for hiking seriously. She decided to take on the Appalachian Trail (AT), which runs 2,190 miles from Springer Mountain, Georgia, to Mount Katahdin, Maine. This hike would set the stage for a life-changing experience, a pursuit that would sustain her for years to come.
A recent breast cancer survivor, Louderback embraced hiking to maintain an active lifestyle. She decided to start with a supported section hike. Supported hikes relieve hikers’ burden of carrying heavy backpacks filled with supplies. Instead, they can trek knowing a van awaits them with the essentials they need. This also allowed her to accomplish her goal while economizing on time—most serious hikers take off six months to hike the AT, not an option for Louderback due to her busy work schedule.
After completing the AT, still her favorite trail, she backpacked other challenging routes, including the Foothills Trail, Tahoe Rim Trail, Benton MacKaye Trail, and the breathtaking John Muir Trail. She also tackled sections of the Collegiate Trail and Pinhoti Trail, and reached the summits of the two highest peaks in the contiguous 48 states.
Emphasizing the importance of preparation and expertise in hiking, Louderback trained to handle extreme conditions. She took a three-day snow basics class to prepare for treacherous trails and completed a wilderness first responder course. She carries a GPS device to contact search and rescue services if needed.
“Whenever I venture onto the trail, I always have it by my side,” she says. “If I find myself in a critical situation, it allows for urgent communication by simply pressing the button and connecting me with help.”
Louderback advises aspiring hikers to start with shorter distances, and says group hikes can provide a safer, more enjoyable experience. She also stresses the importance of informing others about hiking plans, gradually conditioning one’s feet for longer distances, and conducting gear tests to ensure a successful trek.
Louderback’s faith is an essential part of her life, and she feels that God has given her a passion to hike and enjoy the beauty of nature. “Everyone can enjoy the peace and beauty of the outdoors,” she says. “Just get outside."
-By Teresa Hicks
Empowering Medical Education: Active Learning Center launches new era in training
This fall, the Heersink Family Active Learning Center officially launched in the Heersink School of Medicine’s medical education hub, Volker Hall’s Education Tower. Made possible by a philanthropic gift from the Heersink Family Foundation, the Active Learning Center features a “flipped classroom,” where students collaborate in small groups while using screens and digital teaching tools, with the instructor moving between them.
According to Will Brooks, Ph.D., assistant dean for Preclinical Education, active learning is “any instructional method that actively engages the learner in the learning process. It’s contrasted with passive learning, which is more of the lecture style of learning.”

The effectiveness of active learning is backed by research. “Cognitive psychologists and educational theorists have conducted research over the last couple of decades to better understand how people learn efficiently,” says Brooks. “What’s come out of this research is that people across the board learn better when actively engaged in the process and when challenged in some way. Again, contrast that with passive reception—we know that when you sit through a lecture, you retain a very small fragment of that information. When you engage in an active learning session, the retention is much higher.”
The Active Learning Center features 35 tables, each seating six students. Each table has a TV monitor and a microphone. “Instructors can mirror content to all TVs across the room from the lectern computer or their own device, like a phone or tablet,” Brooks says. “Students can also mirror content from their devices to their table’s TV. Microphones allow students who are speaking to the class at large to be heard by the entire room without having topass a microphone around.
 Brooks offers two examples of learning activities medical students will experience in the Active Learning Center. “One that we’ve been using for several years is team-based learning, or TBL, which falls under the flipped classroom umbrella,” Brooks explains. He says flipped classroom methods are ones where the delivery of content is moved out of the classroom for asynchronous, independent student learning—through watching videos or reading a textbook or journal article. Then the classroom is where instructors actively engage students in that material.
Brooks offers two examples of learning activities medical students will experience in the Active Learning Center. “One that we’ve been using for several years is team-based learning, or TBL, which falls under the flipped classroom umbrella,” Brooks explains. He says flipped classroom methods are ones where the delivery of content is moved out of the classroom for asynchronous, independent student learning—through watching videos or reading a textbook or journal article. Then the classroom is where instructors actively engage students in that material.
“In this example, students are given a series of short videos to watch, then when they come into the classroom, TBL has a series of steps,” Brooks says. “The first step is to complete a 10-question readiness assessment individually to self-assess their learning. Then students take the same assessment a second time as a team, working together to answer those same questions and engaging in peer teaching.
“Once those assessments are completed, students spend the rest of the class period working through applications of the information. In the medical school context, they work through a series of clinical cases, working in teams to answer questions and think through the process collaboratively.”
Brooks describes another active learning modality— a form of peer instruction—that will be used starting this year called QAB, which stands for “Questions @UAB.” “Students are again given materials to assimilate on their own, then when they come into the classroom, they work through a series of challenging questions like they might see on their board exams. The questions are multiple-choice, and the students use a polling system to click in what they think is the correct answer. The instructor gets immediate feedback on how much of the class got it right and how many got it wrong.
“If 80 percent or more of the class gets it correct, that’s considered good content mastery and the instructor can move on to the next question. But if less than 80 percent of the class gets it right, the teacher will put the same question up again. This time the students can work together to answer the question and re-poll their responses. Generally, you’ll see an increase in the number of correct responses, verifying the learning process.”
Brooks says these types of active learning methods are not only particularly appropriate for medical education but also a better fit for the current generation of students. “We need our physicians to be able to communicate with each other, with their patients, and with other health care providers, so we want students to develop the communication skills that are a core element of being a physician.
“In addition, today’s learners are all digital natives—they’ve grown up with YouTube and Instagram. They want to have options in how they assimilate information, and they want to do it in their own time. They also have shorter attention spans, that’s just the reality, so we want to take that into account and break up the content into smaller, more digestible chunks.”
A ribbon-cutting ceremony celebrating the launch of the Active Learning Center will take place November 15. Marnix Heersink, M.D., whose $95 million naming gift named the Heersink School of Medicine in 2021, is scheduled to attend, along with Senior Vice President for Medicine and Dean Anupam Agarwal, M.D., medical students, and the school’s medical education leaders, including Brooks.
-By Jane Longshore
Honoring a Special Relationship: A unique connection between a UAB physician and his patient inspires a gift that will resonate for years to come
There are likely many good relationships between doctors and patients at UAB—but few are like the one between pulmonologist Jim Johnson, M.D., and Merritt Pizitz, his patient of 12 years. Pizitz, a prominent Birmingham businessman, made a planned gift to establish an endowed professorship in Johnson’s name in pulmonology. Pizitz said he moved his medical care to UAB more than a dozen years ago and has found the doctors, nurses, clinicians, and other support staff to be highly trained, warm, and helpful. “I have lived in Birmingham for over 80 years, and I think I know Birmingham,” Pizitz says. “When I was young, the lights in the night sky from the blast furnaces west of the city, the horrible 1960s and the city as we see it today. One of the most exciting things during this period was the growth of UAB in Birmingham, located right downtown, with over 20,000 students, 23,000 professional associates, and over 1,500 active physicians. Recently, I decided that I wanted to make a donation to the UAB medical group, but I did not want it to get lost in the [general] funding drive. Therefore, I looked for a way to make a donation that would havesome identity.”
After speaking with Megann Bates Cain, assistant vice president for Development in the UAB Marnix E. Heersink School of Medicine, Pizitz learned that he could direct his gift to a certain department or honor a specific individual.
“I immediately knew what I wanted to do,” he says. “I told her that I wanted to honor Dr. Jim Johnson and name this endowment the James E. Johnson Endowed Professorship in Pulmonary and Critical Care from the funds that will be available upon my death.”
Pizitz said a few years ago he needed a pulmonary specialist and was directed to Johnson.
“Over the years and after many appointments, I learned what a warm, kind, humble, and knowledgeable physician he is,” Pizitz says. “He was only a telephone call away, and Pizitz says, of all of the doctors he’s seen at UAB, Johnson epitomizes medicine of yesteryear: Johnson gave Pizitz his cell phone number and his email address and was instrumental in getting Pizitz follow-up care at the Mayo Clinic for a health issue he faced.
“He is so special,” Pizitz says. “I wanted to honor him for all the things he did for me—for his relationship with me.” For his part, Johnson says he never expected this and tried—unsuccessfully—to convince Pizitz to establish the endowed professorship in Pizitz’s name.
“He wouldn’t hear of it,” Johnson says. “One of his conditions was that it be in my name. It’s a nice thing, a humbling thing—it means that for many years a physician will have my name attached to his or her professorship. I’m humbled and pleased he wanted to do that.”
Johnson, on staff at UAB since 2000, himself is the holder of an endowed professorship, the first Charles and Alice Hohenberg Professor of Pulmonary and Critical Care Medicine. A graduate of Vanderbilt University School of Medicine, Johnson completed his residency in internal medicine and a fellowship in pulmonary and critical care at Brooke Army Medical Center in San Antonio, Texas, and served in the U.S. Army until 2000, including completing a deployment to the Middle East. He retired from the military as a full colonel in 2000 and has been at UAB for 23 years, currently serving as clinical director of the Division of Pulmonary, Allergy and Critical Care Medicine. During his tenure at UAB, Johnson has received numerous awards, including the UAB President’s Award for Excellence in Teaching for the Heersink School of Medicine. Personally, Johnson has been married for 45 years and has five children—all of whom are either in medicine or have served in the military.
Pizitz describes Johnson as warm, kind, and humble and says he wasn’t the only patient Johnson went above and beyond for.
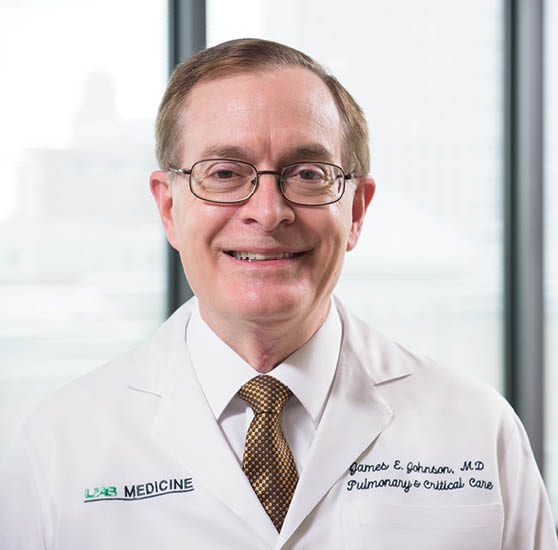 Jim Johnson, M.D
Jim Johnson, M.D
“Jim Johnson is a unique individual and has relationships [like ours] with other people, too,” Pizitz says. “When you have 20 minutes to see a patient, you can only do so much. I almost died about six years ago from a lung issue. I was critical. He was in my room probably two to three times with my daughter. That’s not his job, going to visit patients in their rooms. I had another small event happen, and he called from out of town. He’d already found out about it. He called and talked to me and apologized for not being able to see me. He’s just a special man.”
Johnson returns the respect for his patient, recalling that the pair hit it off from the very beginning.
“He’s one of these guys that’s larger than life,” Johnson says. “When he walks in the room, you know he’s there. He has a big personality and likes to laugh; he always has a joke and a big smile and is glad to see you. He has my phone numbers—my cell number, my office number— but he doesn’t abuse them. If he needs me, he knows how to reach me.”
Johnson says the professorship in his name will help anchor a talented physician to UAB and make the recipient more likely to stay long-term, providing not just salary support but also career enhancement, including taking courses or buying equipment.
“It’s another level of promotion,” he says. “UAB benefits by having that person be better educated and have a salary that is more competitive with other institutions. The benefit is to the individual mainly, but there is a secondary benefit to UAB.”
This gift will make impact for decades, says Mark Dransfield, M.D., director of the Division of Pulmonary, Allergy and Critical Care Medicine.
“This endowment in honor of Dr. Johnson is a terrific recognition of his service to UAB and his patients,” he says. “Jim is well known across the Heersink School of Medicine and UAB Hospital for his excellence in teaching and in patient care. He always goes the extra mile to ensure patients are receiving the best care, both in terms of quality and his attention. This endowment will help us retain and reinvest in our faculty for decades to come and knowing that it was named in his honor will encourage future holders to emulate his caring and professionalism.”
Having an endowed professorship named in one’s honor is a rare distinction for a physician, and Johnson was so moved by his patient’s gesture that, when he found out about Pizitz’s gift, he wrote him a kind letter—by hand, Pizitz points out—and mailed it to him.
“He said, ‘There are over 1,000 doctors at UAB, and I bet you not 4 percent will ever receive this honor,’” Pizitz says. “I still have the letter on my desk, and I’ve considering framing it for my house. It’s so personal, it almost puts tears in your eyes.”
- By Rachel Burchfield
Earliest Influences: Exploring obesity in-utero and how it affects the health of newborns and infants
Researchers at UAB, part of a four-center study analyzing obesity as part of the American Heart Association’s Strategically Focused Research Network, are studying mechanisms and therapeutic targets in obesity.
A summary of this network’s research was published in the Journal of the American Heart Association in February 2023, and includes work from the UAB group suggesting that what happens in the womb could determine whether the offspring will develop obesity or other metabolic diseases later in life.

The center at UAB consists of three groups analyzing the mechanisms of the transgenerational impact of the mother’s obesity and the effects on offspring.
The first group, led by W. Timothy Garvey, M.D., center director, professor with the UAB Department of Nutrition Sciences in the UAB School of Health Professions, and associate director of the UAB Comprehensive Diabetes Center, and Kirk Habegger, Ph.D., associate professor in the UAB Division of Endocrinology, Diabetes and Metabolism, and fellow Rogerio Sertie, Ph.D., looked at how a mother’s diet during pregnancy—whether she ate too much or too little—affected her offspring’s body composition and metabolism.
When mothers were fed a high-fat diet during pregnancy, their offspring had a greater risk of obesity and consumed more food, despite having high levels of hormones that regulate hunger and metabolism.
The study also looked at how the in-utero environment affects the expression of certain genes involved in metabolism and fat distribution, by examining a chemical process called DNA methylation in the brains of the offspring. The researchers found that differences in DNA methylation at specific gene sites are associated with obesity and metabolic diseases in the offspring. These findings provide important insights into how early-life events can impact health later in life and could lead to new ways to prevent and treat these conditions.
Maternal obesity and gestational diabetes mellitus give rise to epigenetic modifications at gene loci affecting insulin and leptin signaling, inflammation, and percent body fat.
The second study group, led by Ashley Battarbee, M.D., assistant professor in the UAB Division of Maternal-Fetal Medicine (MFM), and Lorie Harper, M.D., former UAB MFM faculty, aims to understand how the in-utero environment affects the health of newborns and infants up to 3 months old.
The study enrolled pregnant women who were at or after 36 weeks of pregnancy, separated them into groups based on their weight status and whether they had gestational diabetes, and tested to see whether the differences in the in-utero environment led to differences in the health of their babies. The researchers hypothesized that exposure to maternal obesity, with and without gestational diabetes, during pregnancy has an impact on the metabolic phenotype of infants at 3 months old, leading to increased fat accumulation. They also hypothesized that the same epigenetic modifications associated with cardiometabolic disease traits in older children would also be present at the time of birth. Analyses for this project are ongoing.
The third study group, led by Paula Chandler-Laney, Ph.D., associate professor in the Department of Nutrition Sciences, Bertha Hidalgo, Ph.D., associate professor in the UAB School of Public Health, and fellow Samantha Martin, Ph.D., enrolled mother-child pairs to investigate the effects of maternal obesity with and without gestational diabetes on obesity and cardiometabolic traits in both mothers and children.
The researchers found that mothers with a history of obesity during pregnancy had a poorer cardiometabolic phenotype compared to mothers who had a normal body mass index during pregnancy. However, the severity of this phenotype varied depending on whether the mother also had gestational diabetes. Children’s cardiometabolic traits were modestly correlated with those of their mothers, but only adiposity significantly differed across groups.

The study also looked at the epigenetic signatures of mothers and children ages 4-10. Epigenome-wide association studies found several genes associated with cardiometabolic disease phenotypes, including those involved in leptin and insulin signaling, inflammatory responses, and cellular vesicular trafficking.
The researchers suggest that cardiometabolic health following in-utero exposure to maternal obesity or gestational diabetes may become more pronounced once children reach puberty or adolescence.
Ultimately, the researchers hope to identify modifiable risk factors that can prevent lifelong obesity and cardiometabolic disease in infants with in-utero exposure to maternal obesity and/or gestational diabetes. Together, work from these projects sheds light on the importance of a healthy in-utero environment for the lifelong health of babies and highlights the need for interventions to prevent obesity and related conditions.
-By Adam Pope
A Partnership for Progress: Board of Visitors supports excellence across the Heersink School of Medicine
In 2014, the Heersink School of Medicine engaged a select group of leaders from business, academia, medicine, science, and public policy to form the school’s inaugural Board of Visitors. Nearly 10 years later, members serve as advocates and advisors on Heersink School of Medicine strategy, community engagement, and other initiatives.
In addition to providing insights and expertise, Board of Visitors members have made generous philanthropic investments in the Heersink School of Medicine, totaling more than $134 million. Here we highlight just a few of their many gifts, as well as the lasting impact of their generosity.
In September 2021, a transformational $95 million gift from longtime supporter Marnix Heersink, M.D., named the UAB Marnix E. Heersink School of Medicine. The gift also established two new institutes: the Mary Heersink Institute for Global Health and the Marnix E. Heersink Institute for Biomedical Innovation (learn more on page 28). In addition, having experienced the value of UAB’s medical training firsthand (all of the Heersinks’ children have pursued careers in health care, including three Heersink School of Medicine graduates, a physician/UAB School of Public Health graduate, and a UAB School of Dentistry graduate), the Heersinks made a gift to establish the Heersink Family Active Learning Center, which officially launched this fall (learn more on page 44).
Mary Heersink, who has been married to Marnix Heersink for 45 years and has been a Board of Visitors member since 2017, is an especially passionate advocate for global health, which is also a priority for the school.
“Being a member of the Board of Visitors has allowed me a front-row seat to the extraordinary energy, passion, and creativity that fuels the School of Medicine,” says Mary Heersink. “The focus on the most important emerging forces in medicine and the tangible excitement surrounding the school’s recent successes are contagious. How could one not support the groundbreaking work being done to save lives and improve society?”
For Board of Visitors Co-chairs Gail Cassell, Ph.D., and Ted Love, M.D., supporting the Heersink School of Medicine has involved expanding pathways to medical school through scholarships, among other gifts. "Serving on the BOV has provided me the opportunity me to witness the school’s incredible advancement of research without sacrificing the quality of medical education,” says Cassell. In 2020, she and her husband Ralph Cassell established the Wilkerson-Lacey Endowed Medical Scholarship, named for two important figures from their life. “Our family is pleased to honor Mrs. Lillian Wilkerson and her grandson, Dr. Ontario Lacey. We hope our gift will make it possible for other equally exceptional and deserving young students to fulfill their dreams at this exceptional institution.”
Love established the Love Family Scholarship in 2017 and has supported other programs, including a faculty exchange with the University of Cape Town and the Pittman Scholars Program, which recognizes the achievements of outstanding junior faculty. “UAB is a world-class medical institution, and those who love Alabama should do everything we can to keep UAB Medicine elite,” Love says. “As an African American and an Alabama native, I am proud to support the programs that make UAB Medicine among the best in our nation."
Supporting Heersink School of Medicine deans has been the focus of gifts from two Board of Visitors members. In 2010, James Lee III established the James C. Lee Jr. Endowed Chair for the Dean of the School of Medicine, which has been held by three Heersink School of Medicine deans, including current dean Anupam Agarwal, M.D.
Nancy Dunlap, M.D., Ph.D., completed her internship, residency, and fellowship at UAB and, among other gifts, commemorated her most influential mentors with a gift to the Pulmonary Faculty Development Endowed Fund Honoring Drs. Ben Branscomb, J. Durwood Bradley, William Bailey, and Dick Briggs Jr. “Patient care is demanding, and providing faculty with an outlet for continued learning and career development helps to increase their fulfillment and overall job satisfaction—helping retain the best and brightest at UAB,” she says.
In 2021, Daniel Chu, M.D., MSPH, FACS, an associate professor in the Department of Surgery, was named the Selwyn M. Vickers, M.D., FACS, Endowed Chair in the Department of Surgery, which honors the former Heersink School of Medicine dean. In part because the Board of Visitors was created under Vickers’ leadership, several members contributed to the endowment.
This year, Maryam (Mimi) Head and her daughters Hillery Head and Maye Head Frei, established the first professorship in the Department of Medical Education, the Head Family Endowed Professorship for Medical Education. “I think the Heersink School of Medicine truly is a shining light for Alabama,” says Mimi Head. “It is a place that brings top talent to Birmingham as well as sends its well-trained students everywhere in the country to practice. Investing in this vital institution is an easy choice for me and my family.”
UAB’s patient care and research programs have benefited greatly from Board of Visitors support. Board of Visitors member Mary Battle and her husband William (Bill) Battle III established the Battle Research Acceleration Fund in Rheumatoid Arthritis and the Kayla Smeraglia Single Cell and Cytometry Core Equipment Fund, both of which were inspired by their daughter Kayla Smeraglia’s battle with RA. “At UAB, Kayla received a novel therapy that yielded amazing results,” says Mary Battle. “She continues to do well, is married, has two children and a career. We believe that receiving treatment at UAB made all of this possible.
The couple also established the Mary and Bill Battle Endowed Professorship for Multiple Myeloma in the O’Neal Comprehensive Cancer Center at UAB after Bill Battle was diagnosed with multiple myeloma, a blood-cell cancer. Luciano Costa, M.D., Ph.D., a professor in the Division of Hematology and Oncology, holds the professorship, which is aimed at expanding expertise so patients like Bill can receive care close to home.
Thomas Blount, an original and current Board of Visitors member, established the Jim Straley Endowed Chair in AIDS Research in 2000, which has helped UAB build one of the foremost HIV/AIDS research programs in the U.S. In November 2022, Renee Heffron, Ph.D., who was recruited from the University of Washington to become the director of the UAB Center for AIDS Research (CFAR), was appointed to the chair upon the retirement of longtime CFAR Director Michael Saag, M.D.
Mike Goodrich and his wife Gillian have made numerous gifts to the Heersink School of Medicine. Among them are several gifts benefiting cancer research, including the Gay and Bew White Endowed Chair in Pediatric Oncology, held by Smita Bhatia, M.D., MPH, director of UAB’s Institute for Cancer Outcomes and Survivorship; the Goodrich Family Breast Cancer Research Acceleration Fund; and the Deep South Network for Cancer Control, which works in underserved communities in Alabama and Mississippi to eliminate health and cancer disparities through a network of community health advisors.
William Eugene (Gene) Davenport and his late wife Sandra established the Gene and Sandra Davenport Research Fund in Neurology to support research into progressive supranuclear palsy (PSP), which Sandra battled for 10 years before her death. After undergoing a liver transplant at the Mayo Clinic in Jacksonville, Florida, Gene Davenport also made a gift to support the UAB Liver Center Development Fund.
Former Board of Visitors member Martine Rothblatt, Ph.D., made numerous philanthropic gifts to the school as well as grants through her company United Therapeutics Corporation. Her personal gifts include support for pulmonary arterial hypertension research, inspired by her daughter’s battle with the disease; establishing the United Therapeutics Endowed Professorship in Pulmonary Vascular Disease, held by Suzanne Oparil, M.D.; and a gift to UAB’s Hugh Kaul Precision Medicine Institute.
A grant from United Therapeutics Corporation to UAB’s xenotransplantation program has yielded breakthrough studies, the most recent of which demonstrated, for the first time in a human, that genetically modified pig kidneys provided “life-sustaining kidney function” during the course of a planned seven-day study, while using current standard-of-care immunosuppression drugs.
 The Board of Visitors welcomed three new members this fall: John Gallin, M.D., MACP, Sara J. Finley, and Gordon Lee.
The Board of Visitors welcomed three new members this fall: John Gallin, M.D., MACP, Sara J. Finley, and Gordon Lee.
New Board of Visitors member Sara J. Finley, partnered with family members to establish the Sara Crews Finley, M.D., Endowed Leadership Scholarship. The scholarship honors her mother, Sara Crews Finley, M.D., who co-founded the first medical genetics program in the Southeast with her husband, Wayne Finley, M.D., Ph.D., and served as co-director of the Laboratory of Medical Genetics at UAB for more than 30 years.
In honor of their father, Dr. Wayne Finley, Sara Finley and her brother Randall Finley, M.D., have supported the Reynolds-Finley Historical Library, a collection of over 20,000 rare books, manuscripts, journals, and pamphlets pertaining to the history of medicine, science, and health care dating from the 1300s through the mid-1900s, and the Reynolds-Finley Historical Lecture Series, which explores historical aspects of the health care sciences.
As it enters its second decade, the Board of Visitors will continue to sustain the Heersink School of Medicine’s excellence through its invaluable counsel and transformative gifts.
- By Jane Longshore
Gut Check: New metagenomics study puts gut microbiome at the center of Parkinson’s disease
New research from UAB says the gut microbiome is involved in multiple pathways in the pathogenesis of Parkinson’s disease (PD). The findings, published in Nature Communications, show a wide imbalance in microbiome composition in persons with Parkinson’s disease. The study is the largest microbiome study conducted at the highest resolution, and was selected as one of the journal’s Top 25 Life and Biological Sciences Articles of 2022.
The investigators employed metagenomics, the study of genetic material recovered directly from the stool microbiome of persons with PD and neurologically healthy control subjects.
“The primary aim of this study was to generate a full, unaltered view of the imbalance in PD gut microbiome,” says Haydeh Payami, Ph.D., professor in the Department of Neurology and senior author on the study.
The study reports Parkinson’s disease metagenome is indicative of a disease-promoting microbiome.
“We found evidence for multiple mechanisms that we know are linked to PD, but we didn’t know they were happening in the gut also and are orchestrated by the microbiome,” Payami says.
Investigators found an overabundance of opportunistic pathogens and immunogenic components, which suggest infection and inflammation at play, overproduction of toxic molecules, and overabundance of the bacterial product curli which induces PD pathology, as well as dysregulation of neurotransmitters including L-dopa. At the same time, there was a shortage of neuroprotective molecules and anti-inflammatory components, which makes recovery difficult.
 Haydeh Payami, Ph.D., professor in the Department of Neurology
Haydeh Payami, Ph.D., professor in the Department of Neurology
Payami, who is the John T. and Juanelle D. Strain Endowed Chair in Neurology, and her team enrolled 490 persons with Parkinson’s disease and 234 healthy controls. Just over half of the subjects were male and were predominately older than 50. All were from the Deep South region of the United States, which helped to eliminate confounding by geographic and cultural influence on composition of microbiome.
The researchers studied 257 species of organisms in the microbiome, and of these, analysis indicated 84, more than 30 percent, were associated with Parkinson’s disease.
“Of the 84 PD-associated species, 55 had abnormally high abundance in persons with PD, and 29 were depleted,” Payami says. “We found that over 30 percent of the micro-organisms and bacterial genes and pathways tested have altered abundances in Parkinson’s disease, which indicates a widespread imbalance.”
The study, utilizing the new field of metagenomics, demonstrated an imbalance in the gut microbiome of patients with Parkinson’s disease. At one end of the spectrum, Bifidobacterium dentium was elevated by sevenfold, Actinomyces oris by 6.5-fold and Streptococcus mutans by sixfold. At the other end of the spectrum, Roseburia intestinalis was reduced by 7.5-fold and Blautia wexlerae by fivefold. Overall, 36 percent of PD-associated species had greater than twofold change in abundance, reflecting a 100 percent to 750 percent increase or decrease in PD versus the healthy control group.
“This study created a large dataset at the highest resolution currently feasible and made it public with no restriction to promote open science,” Payami says. “It includes extensive metadata on 490 persons with PD, the largest PD cohort with microbiome data, and a unique cohort of 234 neurologically healthy elderly, which can be used in a wide range of studies. We have shown that there is a widespread imbalance in the Parkinson’s metagenome, creating an environment that is permissive for neurodegenerative events and is prohibitive of recovery.”
As described in the article, “Parkinson’s disease is a progressively debilitating disorder that affected 4 million individuals in the year 2005 and is projected to double to 8.7 million individuals by the year 2030. Although historically defined as a movement disorder, PD is a multi-systemic disease. It is speculated that PD is caused by various combinations of genetic susceptibility and environmental triggers, although no causative combination has yet been identified. The connection between PD and
the gastrointestinal system has long been established.”
“This is exciting research, as metagenomics is a new, albeit fast-evolving field, and the resources, methods, and tools, while state-of-the-art, are still in development,” Payami says. “Undoubtedly more information will be revealed as we increase the sample size and others also conduct metagenomics studies and share the data. We anticipate that in the near future we will have the tools and the analytic power to use metagenomics as a new approach to study PD heterogeneity, search for biomarkers, delve deeper into the origin and progression of PD sub-phenotypes, and investigate the potential in manipulating the microbiome to prevent, treat and halt the progression of PD.”
Co-authors from the UAB Department of Neurology are Zachary Wallen, Ph.D., Guy Twa, Gwendolyn Cohen, Marissa Dean, M.D., and David Standaert, M.D., Ph.D. Other co-authors are Ayse Demirkan, Ph.D., University of Surrey, United Kingdom, and Timothy Sampson, Ph.D., Emory University.
The research was supported by the U.S. Army Medical Research Material Command, the National Institutes of Health, the Parkinson’s Foundation, and Aligning Science Across Parkinson’s through the Michael J. Fox Foundation for Parkinson’s Research.
-By Alicia Rohan
Enabling Discharge with Dignity: Heersink student starts “Compassion Closet” to ensure all patients leave in fresh clothing
 Nik Hakes and a collection point for the Compassion Closet
Nik Hakes and a collection point for the Compassion Closet
A UAB Marnix E. Heersink School of Medicine student has launched a new program to meet a specific need often faced by emergency department patients, particularly trauma patients.
In fall 2022, then first-year medical student Nick Hakes noticed something while shadowing in the UAB Emergency Department—the standard process for treating trauma patients includes removing their clothing, often by cutting it off, to allow first responders or physicians to quickly examine their injuries. Emergency patients’ clothes may also have been damaged or soiled due to a health event. Unless these patients have friends or family who can bring them clean clothes, they leave the hospital in thin paper scrubs.
As a medical student, Hakes was sometimes tasked with cutting a patient’s clothes off. “There have been many times when I silently apologized as I cut off their clothing,” Hakes says.
The solution that Hakes put into motion? A program called Compassion Closet, with a mission to “discharge with dignity,” exemplifying UAB Medicine’s mission of providing patient-centered care.
“Many trauma and emergency department patients are disproportionately affected by social inequalities,” Hakes says. “By advocating for the underserved with action, we can discharge every patient with dignity.”
The Compassion Closet is run out of UAB’s Emergency Department and ensures patients whose clothes have been damaged due to trauma or emergency treatment are discharged from the hospital in clean and weather-appropriate clothing. The closet features new clothing and shoes provided by community donations.
Hakes took inspiration for the Compassion Closet from personal experience. He had a hospital stay in the past, and with no family in the area to bring him a fresh set of clothes, he was discharged in thin paper scrubs, cold and “nearly naked.”
“Trauma can affect anyone, young or old, vigorous or frail, privileged or disenfranchised,” Hakes says. “No matter the circumstances, every patient deserves dignity.”
Formerly, social workers with the emergency department had a few bins of clothing they had donated themselves to provide clothing for patients in need. Now their collection has been merged with the Compassion Closet, which is expanding the effort by providing more space and organization for donations and implementing a check-out process complete with inventory tracking.
“The initial community response was so overwhelming that we created an overflow closet at the medical school,” says Hakes. “Now, the overflow closet itself is overflowing. We have been amazed by the generosity we’ve experienced.” “The Compassion Closet is needed to help the providers of the UAB Emergency Department better meet the basic needs of our patients,” says Todd Peterson, M.D., Department of Emergency Medicine physician and associate dean for Students at the Heersink School of Medicine. “Many of our patients do not have access to clean, adequate clothing to stay warm in the winter months. The Compassion Closet aims to provide these patients with replacement clothing at the time of their discharge from the Emergency Department.”
Jeffrey Kerby, M.D., Ph.D., FACS, director of the Division of Trauma and Acute Care Surgery, says the division is proud to sponsor the initiative by providing funding for the donation bins and closet shelving. He encourages the UAB and local community to rally around the cause and donate new clothing items.

“Many of our trauma patients have their clothing damaged during the course of their injury or care delivery process,” Kerby says. “Life is different in many challenging ways after a traumatic accident or injury, but ensuring our patients have new, clean clothes when they leave the hospital will give them one less thing to worry about as they begin their road to recovery.”
Hakes, who started at the Heersink School of Medicine in the fall 2022 semester, launched Compassion Closet with a team of other medical students: Luke Frost, Bria Gamble, Whitt Harrelson, Gracie Meyer, Anna Musulman, and Jordan Wright. (Two more medical students, Alex Savage and Cole Callahan, have since joined the team.) The students gained insight from physicians, nurses, social workers, administrators, janitors, and—most importantly—patients.
The team got buy-in from stakeholders throughout the Heersink School of Medicine, the Department of Emergency Medicine, the Division of Trauma and Acute Care Surgery, Infection Prevention and Control, and Volunteer Services, who Hakes says all “jumped at the opportunity” to provide even better care for UAB patients.
“In the months the closet has been open, we have helped hundreds of patients and the number of patients benefitting from the closet is only increasing,” Hakes says. “I am blessed to be at an institution where even a medical student can recognize a need, propose a solution, and find enthusiastic support to make an impact.”
- By Allie Hulcher with contributions from Anna Musulman
A Canopy of Care: UAB is leading the way in advancing diabetes research
Carolyn Walsh was traveling on Interstate 459 in Birmingham when she began to feel “off.” She was fighting to stay awake at the wheel, experiencing bouts of severe drowsiness. Before she could pull over, Walsh was in a car accident. Besides a scare, all parties involved were unharmed.
But the accident was a wake-up call. Walsh sought answers to her dangerous drowsiness and received a surprise diagnosis by her general physician: type 2 diabetes. She began medication but had difficulty managing her disease. She finally visited an endocrinologist, who put her on insulin injections immediately, which she notes was the best thing she ever did for her health.
However, Walsh found herself at UAB Hospital-Highlands a few years later when she woke up feeling nauseated, fatigued, breathless, and weak. The team at Highlands quickly recognized that Walsh was facing a potential deadly condition that required immediate treatment: diabetic ketoacidosis. Her cells were not converting blood sugar into energy, so her liver began to break down fat for fuel. A UAB endocrinologist was able to provide a personalized diagnosis: latent autoimmune diabetes in adults, not type 2 as she originally thought.
“Seeing someone who specializes in your specific condition is a smart step in managing your health,” Walsh says. “Having a specialist provide me with the specific latent autoimmune diabetes diagnosis was a game-changer in taking care of myself.”
In 2017, Walsh started receiving nutrition counseling from Amy Warriner, M.D., a professor in the UAB Division of Endocrinology, Diabetes, and Metabolism, which Walsh notes was a critical step in her journey with diabetes.
Now, Walsh, communications director for the UAB Department of Medicine, feels that she is at a manageable place in her disease with her care team’s help. “My connection is very personal. I received lifesaving care here at UAB, and the follow-up transformed how I live with diabetes,” Walsh says. “At every step of the way, people have been rooting for me to be healthy. When I show up in clinic and in the nutrition counseling sessions, they behave like a community of support for me. Absolutely, I’ve got skin in this game, and they do, too. I hope we win the fight together.”
Walsh is one of the approximately 14 percent of adult Alabamians living with diagnosed diabetes. Each year, almost 30,000 adults in Alabama are diagnosed with diabetes, and it is estimated another 120,000 Alabamians have undiagnosed diabetes. The state ranks third in percentage of adults with diabetes and is considered part of the “Diabetes Belt,” a region of the southern United States where people are more likely to have type 2 diabetes than people in other parts of the country.
Given these statistics, UAB and the UAB Marnix E. Heersink School of Medicine have made a priority of understanding diabetes and developing new and better approaches to diabetes care and prevention. The following highlights just a few of the innovative programs housed across the Heersink School of Medicine.
A Milestone in Excellence
2023 marks the 15th anniversary of the UAB Comprehensive Diabetes Center (UCDC), the result of a collaborative effort between UAB, Children’s of Alabama, and supporters in the Birmingham community. The UCDC is composed of over 200 faculty members from 10 different schools and numerous departments, a reflection of the complexity of the disease and the center’s “all hands on deck” approach to understanding the biological mechanisms at work in diabetes and developing new and improved therapies, with the ultimate goal of developing cures.
The UCDC was established in 2008 with a mission to perform cutting-edge research, train future diabetes professionals, and develop novel treatment approaches. The UCDC also serves as the umbrella for various research programs and awards, including the prestigious P30 Diabetes Research Center, U01 Human Islet Research Network grants from the National Institutes of Health (NIH), and several research core facilities.
One of the UCDC’s most promising avenues of research involves a drug called verapamil that was originally developed as a blood pressure medication. Identifying oral verapamil as a potential type 1 diabetes drug was the discovery of UCDC Director Anath Shalev, M.D., a professor in the Division of Endocrinology, Diabetes, and Metabolism and holder of the Nancy R. and Eugene C. Gwaltney Family Endowed Chair in Juvenile Diabetes Research.
This finding stemmed from more than two decades of Shalev’s research into a gene in pancreatic islets called TXNIP. TXNIP is elevated in diabetes and toxic to islets, and verapamil helps bring TXNIP levels back to normal. In 2012, Shalev’s UAB research lab reported that verapamil completely reversed diabetes in animal models, and in 2015 she announced plans to
test the effects of the drug in a human clinical trial.
Type 1 diabetes is an autoimmune disease that causes loss of pancreatic beta cells, which produce insulin. To replace that, patients must take insulin by shots or pump and are at risk
of dangerous low blood sugar events. There is currently no oral treatment for the disease. In 2018, Shalev and colleagues reported the benefits of verapamil in a one-year clinical trial of type 1 diabetes patients, finding that oral administration of verapamil enabled patients to produce higher levels of their own insulin, thus limiting their need for injected insulin to regulate blood sugar levels.
In March 2022, Shalev’s team reported in the journal Nature Communications that use of verapamil to treat type 1 diabetes continues to show benefits beyond one year. Patients taking the medication not only required less daily insulin two years after first diagnosis of the disease, but also showed evidence of surprising normalization of multiple immunological markers.
The beneficial effects of verapamil have now also been independently validated in children with T1D and a large multi-center clinical follow-up trial is ongoing in Europe. A large clinical study from China also demonstrated the benefits of verapamil in the context of type 2 diabetes. In addition, the findings have paved the way for the development of a novel, even more potent and specific TXNIP inhibitor drug and the spin-off of a UAB start-up company (TIXiMED, Inc.) to help move this discovery into patients.
“In humans with type 1 diabetes, even a small amount of preserved insulin production—as opposed to higher insulin requirements—has been shown to be associated with improved outcomes and could help improve quality of life and lower the high costs associated with insulin use,” Shalev says. “The fact that these beneficial verapamil effects persist for two years provides additional support for its potential usefulness for long-term treatment.”
Understanding Diabetes in Minority Youth
The prevalence of type 2 diabetes in youth is increasing in the U.S., primarily among minorities, with Black and Hispanic youth showing the greatest increase. Neither the reason for the increase nor the mechanism underlying the disproportionate risk in minority youth is known.
UAB researchers received more than $3.7 million from the NIH to study the increasing prevalence of diabetes in youth as part of a nationwide consortium. Barbara Gower, Ph.D., interim chair and professor in the Department of Nutrition Sciences in the UAB School of Health Professions, and Ambika Ashraf, M.D., director of the Division of Pediatric Endocrinology and Diabetes at UAB and Children’s of Alabama, are leading the UAB site. UAB is one of 15 institutions selected to participate.
“Our research aims to predict which youth are at greatest risk for developing type 2 diabetes, as well as identify the determinants of progression to type 2 diabetes,” Ashraf says. Preventing the progression to type 2 diabetes is essential. “The knowledge gained from this study would allow us to develop targeted prevention approaches to treat at-risk children,” says Gower.
Over the course of the project, which will end in November 2027, researchers hope to enroll 1,500-3,000 youth who are at risk for diabetes. The main objective of the study is to identify factors that predict conversion to type 2.
All participants will be nondiabetic, but at risk, at the time of recruitment and baseline testing. The team of researchers will assess body composition, continuous glucose monitoring, beta-cell function, insulin sensitivity, diet, physical activity, pubertal progression, psycho-social factors, the intra-uterine environment, and other factors that may affect risk for type 2 diabetes.

Preventing Diabetic Blindness
The leading cause of blindness in American adults is diabetic retinopathy, progressive damage to blood vessels in the light-sensitive tissue at the back of the eye. Yet the source of this damage appears to lie in the belly—mainly a leaky small intestine that weakens the barrier between gut bacteria and the blood system, according to a study published in the journal Circulation Research.
The research blood from human subjects with Type 1 diabetes and a mouse model of Type 1 diabetes were used to explore mechanisms underlying diabetic retinopathy. The results show a way to possibly prevent, or even reverse, the eye damage.
It is known that Type 1 diabetes dysregulates the systemic renin-angiotensin system, or RAS. RAS is a system of hormones and enzymes that regulates blood pressure and other metabolic changes. Besides systemic RAS, there are also local RAS networks that act in diverse tissues. One key RAS enzyme is ACE2, or angiotensin-converting enzyme 2.
The loss of ACE2 in diabetes activates the vasodeleterious RAS axis and lessens the vasoprotective RAS axis. Intriguingly, in a mouse model of Type 1 diabetes, feeding mice with a modified gut bacterial strain of Lactobacillus paracasei, which was engineered to produce human ACE2, protects the mice against diabetic retinopathy progression. Finally, lack of ACE2 in the gut was known to increase gut permeability and systemic inflammation.
The human studies compared people with Type 1 diabetes versus controls. The subjects with Type 1 diabetes were further stratified into three groups: no diabetic retinopathy, non-proliferative diabetic retinopathy, and the more serious disease called proliferative diabetic retinopathy. By measuring levels of certain immune cells and biomarkers in the blood, including gut microbial antigens, the researchers found that human subjects with retinopathy had a dysregulated systemic RAS and profound gut permeability defects that activated components of both the adaptive and innate immune response. Furthermore, increases in the severity of diabetic retinopathy were found to correlate with increased levels of gut permeability biomarkers and a gut microbial antigen. This included increased levels of angiotensin II, the RAS hormone that activates the vasodeleterious RAS axis.
“To our knowledge, this study represents the first time gut barrier disruption has been implicated in the pathogenesis of diabetic retinopathy and also directly links gut leakage with retinopathy severity in human subjects with Type 1 diabetes,” says Maria Grant, M.D., leader of the research team and a professor in the Department of Ophthalmology and Visual Sciences.
Forging New Approaches
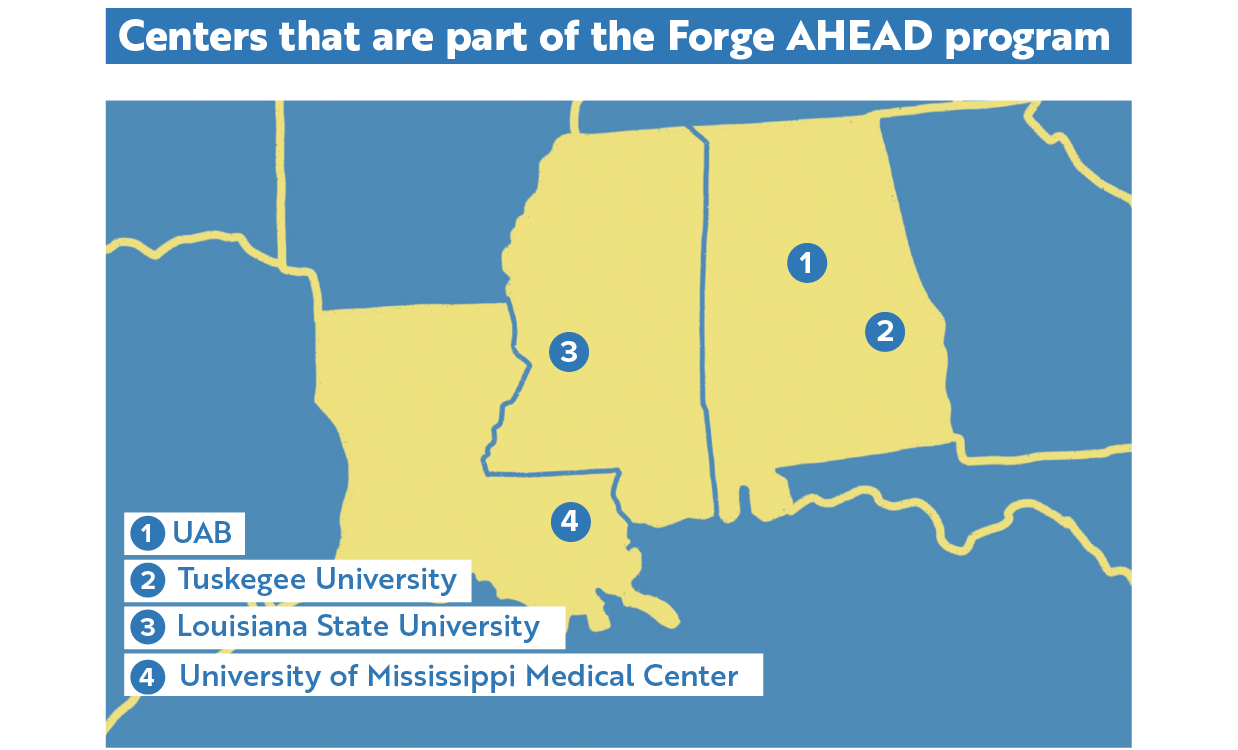
The Forge AHEAD (Advancing Health Equity Across the Deep South) Center was established in 2021 as a collaboration between UAB, Tuskegee University, Louisiana State University System’s Pennington Biomedical Research Center (PBRC), and the University of Mississippi Medical Center (UMMC). The center is funded by the National Institute on Minority Health and Health Disparities with a mission to promote health equity and reduce the burden of cardiometabolic diseases, including diabetes, obesity, and hypertension, among Black Americans and low-income populations in Alabama, Mississippi, and Louisiana.
At UAB, Forge AHEAD is led by Andrea Cherrington, M.D., MPH, professor and interim director of the Division of Preventive Medicine, along with Gareth Dutton, Ph.D., a professor in the Division of Preventive Medicine, and Orlando Gutierrez, M.D., professor and director of the Division of Nephrology. According to Cherrington, the center is made up of an administrative core, a community engagement core that houses a community advisory board and a growing community coalition, and an investigator development core.
The center also supports three R01 level projects. One project that focuses on obesity and diabetes is located in New Orleans and is led by Peter Katzmarzyk, Ph.D., of the PBRC. This clinical study is using patient portals and health coaching to try to improve outcomes. Another project is a community-based study in Alabama and Mississippi that focuses on a combination of peer coaching and community gardens to address obesity, pre-diabetes, and hypertension; the Alabama study is led by Monica Baskin, Ph.D., an adjunct professor in the UAB Division of Preventive Medicine. The third project is led by Tapan Mehta, Ph.D., vice chair for research in the UAB Department of Family and Community Medicine. It is an optimization trial that is recruiting patients in Alabama and Mississippi with poorly controlled diabetes, existing cardiovascular disease, and high levels of social vulnerability. The study is looking at a combination of interventions to improve outcomes that include remote patient monitoring, digital health coaching, and a food delivery service.
“The center has several goals,” says Cherrington. “One is to advance the science around cardiometabolic disparities through these projects. Another big component of the center is focused on growing and diversifying the pool of investigators focused on health equity and health disparities in our region. So we have a scholars program that includes pilot funding for projects for junior investigators, as well as a curriculum that helps provide our investigators with information and skills needed for this kind of work.”
Welcoming Renowned Researchers
In July 2023, the Heersink School of Medicine and the UCDC welcomed renowned clinician-scientists Rita Basu, M.D., and Ananda Basu, M.D., as professors into the Division of Endocrinology, Diabetes, and Metabolism as well as senior scientists in the UCDC and Hugh Kaul Precision Medicine Institute (PMI). In addition, Rita serves as a chair of the UAB Institutional Review Board (IRB) as well as the inaugural medical director of the UAB Office of the IRB, and Ananda serves as the director of the UAB Diabetes Technology Programs.
“As world-renowned researchers, Drs. Rita and Ananda Basu each bring unique and invaluable knowledge and expertise in using sophisticated tracer studies to study type 1 and type 2 diabetes in humans,” says Shalev.
“We are very much looking forward to the many collaborative opportunities that Rita’s and Ananda’s recruitment creates across the center, with the Hugh Kaul Precision Medicine Institute, and across campus.”
After over two decades at the Mayo Clinic, Rita was recruited to the University of Virginia (UVA) in 2017, where she served as a professor in the Division of Endocrinology and the clinical education director of the Center of Diabetes Technology.
Besides serving as a chair of the Mayo Clinic IRB for more than 10 years, Rita was also the associate medical director of the Human Research Protection Program and was responsible for the accreditation of the Mayo health system IRB. At the University of Virginia, Rita was again the IRB chair and made significant improvements and reforms.
Rita serves as the principal investigator on several NIH- and industry-funded projects, including one that seeks to understand insulin resistance in humans that is currently in its 40th year of continuous funding. She has also been an active researcher in the field of non-alcoholic fatty liver disease and has co-authored management guidelines for endocrinologists.
Rita’s work has produced around 175 peer-reviewed publications in scientific journals and has presented more than 150 abstracts in national and International Scientific meetings. She serves on the editorial board of the prestigious American Journal of Physiology as well as the high-impact American Diabetes Association journal Diabetes Care.
Ananda held several leadership positions spanning almost three decades at the Mayo Clinic, and was an endowed professor of medicine as well as a clinical investigator at UVA.
He serves as the principal investigator/co-investigator on multiple NIH projects. His primary research focus is to better understand glucose and glucagon physiology in type 1 diabetes with the ultimate goal to help develop the next generation artificial endocrine pancreas that recreates as closely as possible a truly functional islet. His work also aims to develop a closed loop glucagon infusion therapy to prevent hypoglycemia in patients with post bariatric surgery hypoglycemia syndrome.
As a dedicated clinician, Ananda established a Transplant Endocrine, a Cardio-Metabolic Clinic, and a Diabetes Technology Clinic at the Mayo Clinic. He also led the Mayo Clinic’s Hospital Diabetes Management team for more than a decade while establishing protocols and standardizing care of hyperglycemic hospitalized patients, and dramatically reduced diabetes-related sentinel events during his tenure.
At UVA Health, he set up a similar multi-disciplinary, Diabetes Technology Clinical program to facilitate the use of continuous glucose monitors and closed loop systems for individuals with type 1 diabetes.
Ananda has authored close to 200 peer-reviewed publications in scientific journals and presented more than 150 scientific abstracts in national and International scientific meetings. He has also served on the editorial board of Diabetes Care and as an associate editor of the Diabetes Technology and Therapeutics journal.
Ananda and Rita Basu are world experts in the development of innovative isotope modeling techniques to study whole body human metabolism and physiology. Both are members of the American Diabetes Association, The Endocrine Society, and the American Physiological Society. Division of Endocrinology, Diabetes, and Metabolism Director Fernando Ovalle, M.D., is pleased to have the Basus become part of the division’s clinical research efforts.
“We could not be more excited to have Drs. Ananda and Rita Basu join our growing division,” he says. “I know that Andy will provide outstanding care to his patients and that both Andy and Rita will continue to advance clinical diabetes research at UAB.”
-By Emma Shepard, Jeff Hansen, Caroline Newman, and Jane Longshore
 From left to right: Barbara Gower, Ph.D.,
Ambika Ashraf, M.D., Maria Grant, M.D., Andrea Cherrington, M.D., MPH,
Gareth Dutton, Ph.D., Orlando Gutierrez, M.D., Monica Baskin, Ph.D., Tapan Mehta, Ph.D., Rita Basu, M.D., Ananda Basu, M.D.
From left to right: Barbara Gower, Ph.D.,
Ambika Ashraf, M.D., Maria Grant, M.D., Andrea Cherrington, M.D., MPH,
Gareth Dutton, Ph.D., Orlando Gutierrez, M.D., Monica Baskin, Ph.D., Tapan Mehta, Ph.D., Rita Basu, M.D., Ananda Basu, M.D.
Horizons in ALS Care: UAB’s new ALS clinic offers an eight-to-one advantage
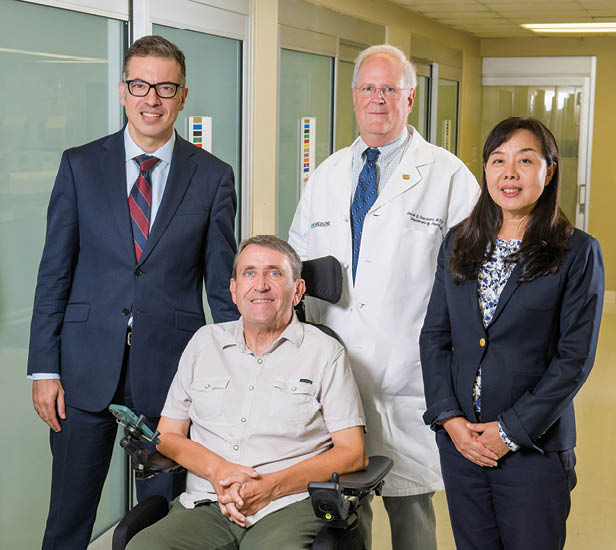 UAB ALS Clinic co-directors Mohamed Kazamel, M.D., and Nan Jiang, M.D. (at left and right), Department of Neurology Chair David Standaert, M.D., Ph.D. (center back), and clinic patient and ALS advocate Kelly Butler (at front).Eight medical professionals. One visit. A new clinic for amyotrophic lateral sclerosis, or ALS, at UAB lets patients see eight health care providers during a single visit, with a single co-pay.
UAB ALS Clinic co-directors Mohamed Kazamel, M.D., and Nan Jiang, M.D. (at left and right), Department of Neurology Chair David Standaert, M.D., Ph.D. (center back), and clinic patient and ALS advocate Kelly Butler (at front).Eight medical professionals. One visit. A new clinic for amyotrophic lateral sclerosis, or ALS, at UAB lets patients see eight health care providers during a single visit, with a single co-pay.
“They’ve got my back,” says Venus Richardson of Mobile, Alabama, who was first diagnosed with ALS in 2019 and began seeing UAB physicians a few months later. “I’ll be making a road trip to UAB every three months now to see the full team. The more you interact with your care team, the better you are able to express how the disease is affecting you. It means better communication and interaction.”
The new clinic is supported by a grant from the Alabama Department of Commerce Innovation Fund. It allowed UAB to expand the existing clinic to see more patients more often. Most patients will come every three months, and during their visit they will interact with their neurologist, physical and occupational therapists, a dietitian, speech therapist, psychologist, social workers, and respiratory therapists. The visit is facilitated by a nurse coordinator with experience working with ALS patients.
“If I have questions or need any information on medications, symptoms, or just questions about diet or lifestyle, they are there to help,” Richardson says. “I think God handpicked the perfect team for me. They take their time to talk to me and listen to me. They don’t just hear me; they listen.”
“The opportunity for patients to see all of their ALS care providers at one visit is a significant benefit,” says clinic co-director Mohamed Kazamel, M.D., associate professor in the Department of Neurology. “Besides convenience and peace of mind for the patient, it allows the care team to work together to build a comprehensive care program for each patient paired with frequent follow-up.”
ALS was identified in 1869 by French neurologist Jean-Martin Charcot, but it became more widely known internationally in 1939 when it ended the career of one of baseball’s most beloved players, Lou Gehrig. For many years, ALS was commonly known as Lou Gehrig’s disease.
The disease affects motor neurons, which reach from the brain to the spinal cord and from the spinal cord to the muscles throughout the body. They govern voluntary movements and muscle control.
ALS causes these motor neurons to degenerate over time until they eventually die. The disease is progressive, meaning the symptoms get worse over time. When voluntary muscle action is progressively affected, people may lose the ability to speak, eat, move, and breathe. ALS has no cure and there is no effective treatment to reverse its progression.
The new clinic opened in January. It sees about 150 patients currently and expects to add about 30 new patients each year. “Beyond expanding our clinical services, the Alabama Innovation Fund grant will allow us to hire an ALS clinical trials coordinator so we can initiate and participate in more national or international clinical trials that shed new light on the disease and may lead to new knowledge about ALS that can point us toward treatments or even a cure,” says Nan Jiang, M.D., Ph.D., associate professor in the Department of Neurology and clinic co-director.
Last year, UAB investigators began enrolling patients in an international trial of a promising new ALS drug. Preliminary studies reported in 2021 indicate the drug, masitinib, may help prolong overall survival. “The 2021 study, which enrolled 394 patients primarily in Europe and South America, showed that masitinib could prolong survival by up to two years as compared with placebo, provided that treatment starts prior to severe impairment of functionality,” says Peter King, M.D., professor in the Department of Neurology and principal investigator for the study at UAB.
The new international study is enrolling more than 400 patients from countries around the world. UAB will enroll 12-15 individuals with mild, early symptoms of ALS. This is the first drug study for ALS at UAB since 2014.
Masitinib inhibits a class of cells called myeloid cells, which includes mast cells, macrophages, neutrophils, and microglia, all part of the human immune system. King was involved in preclinical studies, in collaboration with scientists in Uruguay, showing that Masitinib significantly attenuated inflammatory responses and tissue injury in a rodent model of ALS.
King, along with co-investigators Kazamel and Jiang, says the immune system may contribute to the progression of ALS by doing its job too well. “In ALS, it appears the immune system can be protective in the beginning, but ultimately becomes too active,” King says.
Over the years, King has established a bank of tissues obtained from ALS patients that has allowed him and collaborators to correlate discoveries in animal models with human disease.
“Our work established that there is a robust inflammatory response in peripheral neuromuscular tissues of ALS patients including mast cells, neutrophils, and macrophages,” he says. “Masitinib inhibits the action of these inflammatory cells as well as microglia in the central nervous system by targeting the signaling pathway that activates them. The hope is that dampening the inflammatory response may slow down the progression of ALS.”
-By Alicia Rohan
For more information on the UAB ALS clinic, call 205-934-2120.
A Successful Future on Deck: When thrown a curveball, young patient hits recovery and resilience out of the park
Most children have dreams of what they want to be when they grow up: a doctor, a teacher, a chef. For Waylon Marshall, age 6, being a baseball player has long been a goal.
That dream was threatened in November 2022 when he was in a car accident with his father and sister. In the midst of the crash, Waylon’s left hand got stuck. What happened next is still unknown to first responders and his treating physicians, but Waylon’s pinky, ring, and middle fingers severed on impact, with only two fingers recovered at the scene of the accident.
Waylon was rushed to the emergency department at Children’s of Alabama, where he was met by UAB orthopedic hand surgeon Karlee Lau Loftin, M.D., assistant professor in the Department of Orthopaedic Surgery. Waylon was immediately prepped and sent into a surgery lasting more than 12 hours, where Loftin and team worked diligently to provide vascular function back to his hand while also attempting to reattach his fingers.
“The trauma to his hand was so significant and the force by which the fingers were removed was so great that we discovered successful reattachment of his fingers was not viable; being able to save function of his remaining two fingers and his hand was critical,” Loftin recounts. “ The complexity involved in repairing the trauma in a replantation is often microscopic, as we saw in Waylon’s case, but operating on a patient of his size increases that challenge.”

Waylon’s mother, Dena Marshall, could not help but fear what this accident would mean for her son’s life. “You just wonder about all the ways this would impact and shape his life and, of course, how he would respond to this traumatic event; he is so young,” Dena shares. “And naturally, we thought about how this would impact his passions like his love of playing baseball. He was left-handed, and that injury was certain to impact his ability to throw and catch. We just didn’t know what this all would mean and how he would react.”
But within days, both Loftin and Dena were stunned by Waylon’s progress and resilience. As he took his injury in stride and with a maturity not found in most children, both acknowledged his fighter spirit and determination to live a fulfilled life that would not be impacted by this accident.
“I have been blown away by how Waylon has taken responsibility at such a young age for his own life. He has not pretended that this wasn’t happening to him but rather made up his mind that this injury would not limit him,” Loftin says. “He set goals in his mind and has worked hard to meet them.”
In just a few months’ time, Waylon’s forward-facing mindset was evident: He had already learned to catch with his new left hand and throw with his right—the opposite of how he played prior to his accident—and rivaled his tenacity on the field with his determination at regular hand therapy appointments.

“Waylon is just such a cool patient—he’s our little daredevil. He is so motivated and fiercely independent, and the entire clinic lights up when he walks in,” says Waylon’s hand therapist Christy Mann, OTR/L, CHT. “He is so focused on using that hand and has not once ever neglected it. His fingers were super sensitive when we began; but we do specific exercises that help with texture exposure so that, when he puts his hand in the baseball glove, he has positive and normal sensations.”
Loftin notes that part of Waylon’s medical success is due in part to being cared for at a Level I trauma center like UAB’s. The extent of his injuries was so extensive and specific that being cared at a place like UAB made a critical difference.
“At UAB, we specialize in replantation and microvascular surgery just like Waylon had, and we have board-certified hand surgeons who do this day in and day out,” Loftin explains. “It’s not a service that you could find everywhere in Alabama, so I feel fortunate that Waylon made it to us here at UAB for care and in a time frame that allowed us to help him.”
-By Savannah Koplon
Incubating Innovation: New institutes are forging collaborations and fostering novel ideas to address health care challenges at home and across the globe
Connection is one of the most powerful forces shaping our world today. Connections between people, communities, institutions, and nations are the building blocks of change, and are essential to innovation and transformation in medicine and health care. In 2021, UAB experienced a historic turning point when Marnix Heersink, M.D., a renowned eye surgeon, innovator, and entrepreneur, gave a $95 million gift—the largest in the university’s history—to name the UAB Marnix E. Heersink School of Medicine. In addition, the gift established two new institutes in priority areas for the school: the Marnix E. Heersink Institute for Biomedical Innovation and the Mary Heersink Institute for Global Health. In the years since, both institutes have worked to forge connections—between physicians, researchers, and experts nationally and internationally to advance knowledge, and via technologies through which data and information can be shared. In this story, we explore how both institutes have begun to meet their missions and are laying the foundation to make lasting and meaningful change to improve health care and health outcomesacross the state and the globe.
Boosting Biomedical Innovation
The Marnix E. Heersink Institute for Biomedical Innovation aims to drive the transformation of health and health care by future-proofing the health care workforce and fostering and facilitating innovation that will improve health outcomes and economic development.
Led by Rubin Pillay, M.D., Ph.D., assistant dean for Global Health Innovation in the Heersink School of Medicine and chief innovation officer for the UAB Health System, the Heersink Institute for Biomedical Innovation focuses on entrepreneurial health care innovation initiatives that foster and facilitate health care and socioeconomic transformation.
According to Pillay, the health care system needs significant cost, quality, access, and productivity improvements. “While medical treatments have made astonishing advances over the years, the packaging and delivery of treatments are often inefficient, ineffective, and not consumer-friendly,” says Pillay. “The problems, ranging from medical errors to the soaring cost of health care, beg for innovative solutions involving every aspect of health care—its delivery to consumers, its technology, and its business models.”
The Marnix E. Heersink Institute for Biomedical Innovation was established to combat these gaps in health care through education, research, and applied activities. “The institute is bringing together complementary skill sets to enhance the transformative power of teaching and learning in biomedical innovation and accelerate high-value, innovative solutions through the continuum of discovery, translation, and application, in partnership with the clinical practice at UAB and other local and international partners,” says Pillay.
 Marnix E. Heersink Institute for Biomedical Innovation team members (clockwise from top left) Carlos Cardenas, Ph.D., Rubin Pillay, M.D., Ph.D., Deneka Henry, Jose Flores, Tara Black, and Carlon Harris.
Marnix E. Heersink Institute for Biomedical Innovation team members (clockwise from top left) Carlos Cardenas, Ph.D., Rubin Pillay, M.D., Ph.D., Deneka Henry, Jose Flores, Tara Black, and Carlon Harris.
The institute is anchored by several internal and external partnerships, including UAB’s Bill L. Harbert Institute for Innovation and Entrepreneurship, Collat School of Business, and Schools of Health Professions and Engineering, as well as McMaster University in Hamilton, Ontario, Canada.
To expand on its strategic focus areas—education and training, innovation infrastructure, and internal and external partnerships—the institute has been active in establishing educational program offerings, hosting symposiums and grand rounds, and growing partnerships through various events and meetings.
One of the institute’s first initiatives was to begin offering educational programs aimed at broad audiences, allowing anyone interested in innovation in health care to participate. “We want to futurize health care by developing a cadre of health sector employees—both clinical and non-clinical—who are creative, innovative, and entrepreneurial,” says Pillay.
“The institute has an opportunity to offer this innovation education and training.”
Currently, the institute offers two certificate programs that prepare participants for careers in dynamic health care sectors by fostering creativity, innovation, and entrepreneurship.
The institute’s Artificial Intelligence (AI) in Medicine Graduate Certificate provides solid foundations in the understanding and application of AI as well as the safety, security, and ethics of using AI to improve the health and lives of patients. The institute also offers a Digital Healthcare Graduate Certificate that provides an educational foundation of the digital landscape in health care.
In 2022, the Heersink Institute for Biomedical Innovation, in partnership with UAB Medicine, launched its Healthcare Innovation Academy, a program for health care professionals to optimize their teams’ quality, access, and solutions through creativity, innovation, and entrepreneurship.
“By definition, innovation is an applied activity ..." and this is reflected in our approach,” says Pillay.
“Our research and practice reflect and help us better understand competencies, pedagogy, and organization that best foster and facilitate innovation in health care settings.”
This approach is also evident in the institute’s engaging events. The institute regularly hosts symposiums and grand rounds, inviting participants to learn about Healthcare 3.0, Disruptive Technology Empowering Precision Health (D-TECH, one of the Heersink School of Medicine’s four strategic research focus areas), and other topics. These events and presentations are hosted between larger symposiums and seminars to engage audiences, both internal and external to UAB, and to allow opportunities for participants to learn more about health care innovation.
Since its establishment, the institute has also held several larger events, including an AI in Medicine Symposium, Digital Health Symposium, and the United States’ first Metahealth Symposium, which was held in person and in the metaverse, an emerging 3D-enabled digital space that uses virtual reality, augmented reality, and other advanced technology to allow people to have lifelike experiences online.
Through these events, the institute aims to increase awareness of the need for innovation in health care while providing educational opportunities to ensure that health care organizations have a critical mass of individuals who understand the innovation imperative and process.
Marnix Heersink, M.D., says it has been exciting to witness the growth of the institute that bears his name. “The evolution of the institute has been remarkable from my family’s perspective,” he says.
“To think that so much has happened in such a short period of time is very inspirational. There is so much opportunity for making lives better, and our hope is that the momentum created with the Biomedical Innovation Institute will make an impactful, sustainable difference for many.”

Embracing Global Health
Many Heersink School of Medicine clinicians, researchers, and students have been involved with global health work through the years, but in September 2021, the Mary Heersink Institute for Global Health (MHIGH) was established to create a hub for the school’s multifaceted global health efforts. With a commitment to research, education, service, and collaboration, the institute is working to improve overall health and well-being and promote equity in health outcomes on a global scale, particularly in underserved regions around the world, including the U.S.
“UAB’s global health program already had a solid framework built on transnational collaboration and creative thinking; its potential and curriculum are now being thoughtfully expanded,” says Mary Heersink, an advocate for global health and food safety and a longtime member of the Heersink School of Medicine’s Board of Visitors. “I believe that international collaborations will increase so that graduates, educators, researchers, and students may maximize their influence on a truly global scale.”
“We promote a decolonized approach to global health, meaning our initiatives offer equal or even greater benefit and leadership opportunities to our collaborators as we address shared priorities,” says Alan Tita, M.D., Ph.D., director of the institute and associate dean of Global and Women’s Health. “Our goals are not meant to be solely focused on us or our own good, but on shared health problems of our interconnected populations for mutual benefit.”
Faculty members and researchers at UAB are engaged in a wide range of studies and initiatives focused on global health challenges, such as infectious diseases, maternal and child health, and noncommunicable diseases, including cancer, that contribute to scientific knowledge and inform evidence-based interventions and policies. MHIGH has provided six pilot grants to UAB faculty and global collaborators to catalyze these types of studies and initiatives and provide experiential opportunities for trainees in the U.S. and partner countries. In addition to providing pilot funding, the MHIGH team members are personally involved in
global health research.
 Mary Heersink Institute for Global Health team members (clockwise from top left) Penny Whiteside, MPH, Lynn Matthews, M.D., MPH, Alan Tita, M.D., Ph.D., Eric Wallace, M.D., Michelle Feese, MPH, Matt Heimann, M.D., and Michelle Lee.
Mary Heersink Institute for Global Health team members (clockwise from top left) Penny Whiteside, MPH, Lynn Matthews, M.D., MPH, Alan Tita, M.D., Ph.D., Eric Wallace, M.D., Michelle Feese, MPH, Matt Heimann, M.D., and Michelle Lee.
The Chronic Hypertension and Pregnancy (CHAP) trial received the Clinical Trial of the Year award for 2023 from the Society of Clinical Trials. This significant achievement recognizes the trial’s success and highlights the remarkable contributions of Tita, the trial’s lead investigator.
Tita’s research has focused on maternal-fetal medicine and improving pregnancy outcomes. His insights and leadership played a vital role in shaping the trial’s design to examine the impact of hypertension on pregnant women and their babies and its potential implications for maternal health. Collaboration across UAB and multiple institutions was crucial.
“Chronic hypertension causes serious and life-threatening complications for pregnant women and their babies,” says Tita. “Between 70 percent and 80 percent of pregnant women with chronic hypertension fall into the ‘mild’ category, where there was no medical consensus for treatment.”
The CHAP Trial produced remarkable results, demonstrating that the intervention strategy using appropriate medications during pregnancy significantly reduced adverse maternal and newborn events. This groundbreaking finding has had an immediate impact on treatment in the U.S. and has the potential to transform the management of hypertension and improve maternal, newborn, and cardiovascular health globally.
For this study, Tita also was recognized during the Clinical Research Forum’s annual Top Ten Clinical Research Achievement Awards, receiving the organization’s most prestigious honor, the Herbert Pardes Clinical Research Excellence Award.
MHIGH recognizes the importance of equipping future health care professionals with the knowledge and skills to address global health challenges. This year, the institute partnered with the UAB School of Public Health to develop the UAB Master of Science in Global Health (MSGH), the first degree of its kind to be offered by a university in Alabama, advancing the study of global health through the lens of health equity. This program aims to provide students with a comprehensive understanding of global health issues and prepare them to make meaningful contributions in their future careers. In an effort to foster international collaboration and further partnerships, UAB will be part of a global health consortium that will expose MSGH students to shared graduate courses.
“We hope to welcome trainees from diverse local and global backgrounds, including underrepresented groups and low- and middle-income countries, who will become leaders in global health,” says Matthew Heimann, M.D., associate director for Education at MHIGH and co-director of the MSGH program.
Funding from the NIH/Fogarty International Center and the Bill and Melinda Gates Foundation, in addition to partnerships with regional organizations, enable UAB to leverage expertise, resources, and networks to make a broader impact on global health outcomes.
“As a new institute, we are strengthening existing partnerships and forging new ones as we expand opportunities for faculty, staff, and trainees to engage in global health,” says Tita.
MHIGH has hosted multiple seminars with partners from different regions sharing their knowledge and collaborated with other UAB and global entities to host its first symposium, the UAB Global Health Symposium: Promoting Equity in Global Partnerships, September 28-29, 2023. A highlight of the symposium was the inaugural Dr. Michael Saag Lecture, presented by Roger Glass, M.D., former director of the NIH John E. Fogarty International Center and NIH associate director for International Research.
The symposium also featured panel discussions, lectures, and networking opportunities, creating a dynamic environment for sharing insights and fostering interdisciplinary collaboration. By bringing together experts from diverse backgrounds, the UAB Global Health Symposium serves as a catalyst for addressing equity and advancing research, education, and training collaborations to identify sustainable solutions to improve health outcomes worldwide.
By fostering interdisciplinary partnerships and service initiatives, conducting groundbreaking research, and training the next generation of global health leaders, MHIGH aims to be a beacon of hope and progress in the pursuit of improved health outcomes here in the U.S. and globally.
Propelling Partnerships
In addition to naming the Heersink School of Medicine and establishing the new institutes, the Heersink gift connected UAB to an exciting collaborative partner, McMaster University in Hamilton, Ontario, Canada. Marnix Heersink made philanthropic investments to establish biotech commercialization hubs and global health institutes at the two universities.
The parallels between the two institutions are many. Like UAB, McMaster is a leader in health professions training. Both UAB and McMaster are research-intensive public universities and are similar in size, with excellent affiliated medical centers. Just as UAB has pioneered numerous advances across our mission areas, McMaster has spearheaded innovations in education, research, and care, including originating problem-based learning in medical education and evidence-based medicine.
Another similarity: UAB and the Heersink School of Medicine are nationally recognized for expertise and leadership in health equity and health disparities research and programming, thanks in large part to the diverse population of Birmingham and Alabama, while McMaster serves a large Indigenous population that traditionally has been underserved in health care and underrepresented in research.
Each institution has hosted the other’s leaders to begin outlining collaborative opportunities. On March 16, 2022, the Heersink School of Medicine hosted Marnix and Mary Heersink as well as McMaster University President David Farrar, Ph.D., and Faculty of Health Sciences Dean Paul O’Byrne, M.B., B.Ch., BAO. The itinerary included a tour of Volker Hall, UAB’s medical education hub, and a drive-by of the future site of the Altec/Styslinger Genomics Building and the Marnix E. Heersink Biomedical Innovation Conference Center. The visit also included meetings with UAB President Ray Watts, M.D., and Heersink School of Medicine senior leaders, as well as Pillay, Tita, and Suzanne Lapi, Ph.D., professor and vice chair of Translational Research in the Department of Radiology and the UAB Cyclotron Facility director.
On June 29, 2023, McMaster University hosted Marnix Heersink as well as a delegation from UAB that included Heersink School of Medicine Senior Vice President for Medicine and Dean Anupam Agarwal, M.D.; UAB Provost and Senior Vice President for Academic Affairs Pam Benoit, Ph.D.; UAB School of Public Health Dean Paul Erwin, M.D., DrPH; UAB School of Health Professions Dean Andrew Butler, Ph.D.; and Pillay, Tita, and Lapi.
The meetings were a chance for both institutions to highlight their innovative programs in global health, women’s health, health care innovation and commercialization, and radiopharmaceuticals and medical imaging. In addition to the vast potential for research and clinical trial collaborations, participants discussed opportunities for faculty and student exchanges and shared certificate and other educational programs and symposia.
Closer to home, the Heersink gift has also spurred collaboration with city, business, and health care leaders in the Heersinks’ hometown of Dothan, Alabama, initiatives that will expand UAB’s impact on health and health care in the southern part of the state. In particular, the Heersink Institute for Biomedical Innovation launched the Community Entrepreneurship Initiative in Dothan in March 2023. Poverty is one of the leading causes of health disparities in the U.S., and this 12-month intervention program aims to help local entrepreneurs from disadvantaged backgrounds improve their circumstances and improve overall healthy living conditions for themselves, their families, and their communities.
On another front, Chris Brainard, FACHE, senior director of the UAB Medicine Office of Patient Experience, hosted an Innovating the Patient Experience program in Dothan in April 2023. The program teaches local health care leaders how to future-proof their organization by building a reputation as a leader in human-centric health care. Participants learn the tactics and strategies that have helped top health care organizations differentiate their brands by becoming leaders in patient care experience and employee engagement. The event helped participants equip their teams with human-centric approaches to elevate performance and innovate rapidly.
In the two-plus years since the Heersink Institutes were established, firm foundations have been laid for powerful impact in biomedical innovation and global health. The momentum continues to build as new programs are introduced, each one forging new connections that will advance the Heersink School of Medicine’s excellence in research, education, and patient care.
-By Emily Johns, Jane Longshore, and Shawna Masters
Called to Serve: Faculty and staff veterans share how their military experiences shaped their careers in health care
The path to a career in medicine and health care is unique for every person. For some, the first spark of interest occurred while they were answering the call for a different kind of service in the military. In advance of Veterans Day, UAB Medicine magazine talked with several military veterans at the UAB Heersink School of Medicine to learn how their time in the armed forces impacted their professional lives and their journeys to medicine. With a unique blend of experience, dedication, and compassion, they continue to make a profound impact on the lives of others, embodying the true spirit of sacrifice.
Building Military-Civilian Partnerships
In 1999, Jeffrey Kerby, M.D., Ph.D., left UAB to join the military. When he returned to UAB four years later, he brought the military with him.
A Missouri native, Kerby originally came to UAB after earning both his undergraduate and medical degrees from the University of Missouri at Kansas City. He earned a Ph.D. in Biochemistry and Molecular Genetics from UAB in 1997, then completed his surgical residency.
In order to further his medical training, Kerby joined the United States Air Force under the Health Professions Scholarship Program. In doing so, Kerby was continuing a family tradition. His father served in the Navy during the Korean War, and his older brother spent 23 years as an Air Force fighter pilot.
During his time in the Air Force, Kerby made the connections and learned the skills that eventually led to the formation of military training programs at UAB, including the Special Operations Surgical Team (SOST), a permanently stationed group of active-duty Air Force personnel who work at UAB’s Level 1 Trauma Center.
“Serving in the military was the most important time in my career as far as the people I met and the relationships I developed,” says Kerby, who currently serves as the Brigham Family Endowed Professor in Trauma and Acute Care Surgery and is the director of the Division of Trauma and Acute Care Surgery. “It definitely led to the collaborations we’ve been able to establish with the Air Force at UAB.”
The connections started during Kerby’s time at Wilford Hall Medical Center, located on the grounds of San Antonio’s Lackland Air Force Base. The center contained a verified trauma program that also served the civilian population.
While there, Kerby began working with the head of the trauma program, Donald Jenkins, M.D., on the development of small, mobile surgical teams that could be utilized in combat situations. Each team consisted of a trauma surgeon, orthopedic surgeon, scrub tech, anesthetist, and emergency medicine physician.
“The idea was for these small teams to be able to go far forward into a conflict, set up an operating room in a shelter of opportunity—a shed or a tree with a canopy—and establish a mobile OR to provide stabilizing damage-control surgery for injured combatants close to the front lines,” Kerby says.
Two years of planning and training were suddenly put to the test following the 9/11 terrorist attacks in 2001 and the ensuing conflicts in Afghanistan and Iraq.
“You always want to avoid those circumstances,” says Kerby, who was deployed in 2002 in support of Operation Enduring Freedom. “But given the need at that time, we were glad we had developed the teams and gone through the training and were ready to utilize that resource for the soldiers who were putting themselves in harm’s way.”
Kerby was able expand upon that work once he returned to UAB in 2003 following his departure from the Air Force, where he achieved the rank of lieutenant colonel. First, in 2006, Kerby used his military connections to bring an Air Force Pararescue Jumper (PJ) training program to UAB.
“They do rescues for downed pilots and anybody who needs to be extricated from a situation. They also serve a tactical role for specialized missions” Kerby says. “They’re already highly trained combat medics, but they need to maintain their trauma life-saving skills. When the opportunity presented itself to develop that program at UAB, I jumped at the opportunity to support this military mission in my new civilian role.”
The program initially trained approximately 50 Air Force personnel each year, but Kerby says it has expanded significantly in recent years thanks in part to the efforts of Daniel Cox M.D. In addition to being chief of UAB’s Trauma Service and an associate professor in the Division of Trauma and Acute Care Surgery, Cox is a 13-year Air Force veteran who still serves in the Air Force Reserves.
Under the direction of what is now called the Special Operations Center for Medical Integration and Development (SOCMID), the program will eventually train 300 to 400 personnel each year. “It’s turned into a total-force operation for trauma training for these Air Force PJs,” Kerby says.
UAB’s success with the original 2006 PJ program led to the establishment of the SOST program in 2010. Under the program, active-duty Air Force surgeons are credentialled to work at UAB’s trauma center, where they often encounter injuries similar to the type they might see on the battlefield.
“We now have four SOST teams stationed here taking calls in our trauma units, but they’ll also deploy as a team wherever they’re needed around the world,” Kerby says. “Building this military-civilian partnership at UAB and seeing it flourish and grow has been one of the most rewarding aspects of my career.
“The great thing about doing this at UAB is the collaborative spirit that’s part of the culture here. When we first started talking about this military-civilian collaboration and how it would need multi-departmental assistance, everybody was fully supportive of the idea. I never had a leader say no. It was always, ‘How can we get to yes.’ That’s what’s so special about UAB.”
 Rosylen Quinney's service with the Army Reserves Military Police in Iraq spurred her to consider a career in health care.
Rosylen Quinney's service with the Army Reserves Military Police in Iraq spurred her to consider a career in health care.
From Military to Maternity
After experiencing death up close as a young Army Reserves recruit, Rosylen Quinney decided she wanted to pursue a career dedicated to the creation and preservation of life. She currently is doing just that as a Clinical Research Coordinator II in the Heersink School of Medicine’s Center for Women’s Reproductive Health.
A native of Forkland, Alabama, Quinney graduated from Demopolis High School in 1987, then began a 10-year stint with the U.S. Army Reserves 1165th Military Police Unit. At the time, she envisioned that her military service would lead to a career in civilian law enforcement.
But in 1991, Quinney was deployed to Iraq for six months as part of Operation Desert Storm. While there, Quinney says she witnessed things “that a young woman from Greene County never could have imagined.” This included watching as one of the sergeants in her unit stepped on a landmine and died.
“It’s obviously something I will never forget,” Quinney says. “At first, I wanted to go into police work. But after being deployed and seeing all the death, I made up my mind while still there that I wanted to come home and be a nurse. That’s how my career changed from being a law officer to being in the medical field.”
It took more than two decades, but that decision eventually brought Quinney to UAB. She began her medical career in 1993 by working at a Birmingham senior-living facility and becoming a Certified Nursing Assistant. She then furthered her training through a program at Carraway Methodist Medical Center for Intensive Care Technicians.
In 2000, Quinney began working as a Clinical Medical Assistant with Alabama Neurology Associates, which is where she first became interested in the research side of the profession. That led to a series of roles as a Clinical Research Coordinator for several facilities, including the Birmingham Pain Center and St. Vincent’s Central Research Associates.
Quinney assisted on numerous clinical trials during that time, gaining experience in investigational drugs, medical devices, biologics, vaccines, surgical intervention, and other treatments and procedures.
Through it all, Quinney says she continually monitored potential job openings at UAB, where both her brother and sister-in-law previously worked. So when she received an offer in 2018 to join the Heersink School of Medicine’s Department of Obstetrics and Gynecology in the Division of Maternal Fetal Medicine, she jumped at the opportunity.
“I had never done OB/GYN or neonatal research, but as soon as I interviewed here, I knew this is where I should be,” Quinney says. “I just fell in love with the babies and the moms. Especially the babies.”
Quinney currently is co-coordinating the Randomized Trial of Continuous Airway Pressure for Sleep Apnea in Pregnancy study with the national Maternal Fetal Medicine Units Network out of George Washington University. She serves as lead coordinator on the Identifying and Assessing Multi-Level Barriers to Equitable Postpartum Sterilization study and The Meaning of Screening Intervention Study which is evaluating the effectiveness of a prenatal screening educational game to improve knowledge and reduce decisional conflict among underrepresented and a range of health literacy levels of pregnant people.
 Rosylen Quinney was awarded the National Defense Service Medal for her service in Iraq during Operation Desert Storm.
Rosylen Quinney was awarded the National Defense Service Medal for her service in Iraq during Operation Desert Storm.
But her primary passion is working as the program manager for the P3 Providing an Optimized and emPowered Pregnancy for You (P3OPPY) study, funded by the American Heart Association.
UAB is the coordinating center for the P3 EQUATE Network, which is a collaborative effort between research institutions and community
partners aimed at improving maternal and infant health outcomes. The study is being led by Rachel Sinkey, M.D., an assistant professor of Obstetrics and Gynecology at the Heersink School of Medicine, and Pediatrics professor Wally Carlo, M.D. The focus is on reducing health disparities among maternity patients, particularly for Black and underserved populations.
“We’re trying to see why African American women have the highest maternal mortality rate in the U.S., and why they have so many health disparities,” Quinney says. “I’m writing proposals, creating data files, facilitating meetings. I’ve learned how to do all that during the time I’ve been at UAB. I probably wouldn’t have the opportunity to be doing this if I wasn’t at UAB.”
Quinney says her years in the military taught her traits that she utilizes in her current role, including “how to be disciplined and pay attention to the smallest of details in order to execute my assignments.”
Of course, the smallest details that she enjoys the most are the babies who are benefiting from her research work. Welcoming newborns into the world is a long way—both figuratively and literally—from the Iraq experience that sent her down the medical path.
Challenges and Rewards
Most medical treatments and procedures are focused on curing the body, but for Pete Lane, D.O., his work is also about repairing the spirit.
Since 2004, Lane has been the medical director of Addiction Medicine in the Department of Psychiatry and Behavioral Neurobiology. In that role, he has witnessed the transformative power of successful addiction treatment.
“Nowhere in medicine that I’ve been have I seen a field where I can have such a huge impact on a person’s quality of life,” Lane says. “They transform physically, socially, and spiritually through the recovery process. If you take a photo of them when they get here and again when they depart, they don’t even look the same. Being able to watch somebody transform and grow into a sober person in recovery is hugely gratifying.”
A native of rural upstate New York, Lane became interested in medicine after enlisting in the Army in 1980. He says there was a shortage of medical lab technicians, so he volunteered and was sent to Redstone Arsenal in Huntsville for training.
“I became interested in the lab tests, where you’re looking at the biology of whatever problem the patient is going through,” Lane says. “I learned a lot about these tests, how to use them and what they mean. That got me interested in being able to diagnose a medical illness, which led me into wanting to go to medical school.”
Lane received his undergraduate degree in biology from the University of Alabama at Huntsville in 1988, graduated from Kirksville College of Osteopathic Medicine in Missouri in 1994, then completed a Family Medicine residency at UAB in 1997. He worked in private practice for a few years while serving as a volunteer faculty member at UAB before joining the Heersink School of Medicine full-time in 2001.
Over the past two decades, Lane has experienced the ups and downs of working in addiction treatment. Despite all the efforts to treat the disease, Lane says, “We’re still seeing a growing population that’s homeless and using substances.”
That is particularly true for military veterans. According to the U.S. Department of Veterans Affairs, approximately 11 percent of vets who visit a VA facility for the first time are dealing with some sort of substance use disorder, a figure that is slightly higher than the general population.
“We need more people to get involved and to help treat this patient population,” Lane says, “as well as make changes above our level to hopefully eliminate this problem.”
But Lane also knows what is possible when a person suffering from addiction successfully experiences recovery. And that, he says, is what makes his role at UAB so rewarding.
“Sure, they’re not the most pleasant people to deal with at times, particularly when they’re intoxicated or in withdrawal. But once they’re sober, they’re just regular people,” Lane says. “There are some who you just can’t change. But for a lot of them, if you treat them appropriately and get them a safe discharge plan, then they’re not coming back.
“It’s really satisfying to see somebody totally change their life and be there for their family, go back to work, and be successful at life. That’s what I try to help them do.”
-Story by Cary Estes, Photography by Andrea Mabry
Celebrating 70 Years of Veterans’ Care
On March 16, 1953, the Birmingham VA Health Care System (BVAHCS) opened its doors in the historic Southside district of Birmingham. Today, the medical center is a level 1A acute tertiary medical and surgical care center with 10 community-based outpatient clinics located in Anniston-Oxford, Bessemer, Childersburg, Guntersville, Gadsden, Huntsville, Jasper, Shoals, and two in Birmingham. The health care system employs more than 3,000 staff members that serve over 71,000 veterans in Alabama. On March 16, 2023, the Birmingham VA Health Care System celebrated 70 years of service with a special ceremony. The Heersink School of Medicine is the primary clinical affiliation and longtime partner of BVAHCS. Each year almost 700 Heersink School of Medicine residents rotate at BVAHCS, and over 115 medical students rotate at BVAHCS each academic year. In addition, research at the BVAHCS is conducted in collaboration with UAB scientists. Grants funded through the VA support numerous clinical and basic science research projects.– Emily Smallwood
A Leader's Journey: Dean Anupam Agarwal reflects on his path to UAB and shares his vision for the future
On February 3, 2023, a new era in the history of UAB began when it was announced that Anupam Agarwal, M.D., was named senior vice president for Medicine and dean of the UAB Marnix E. Heersink School of Medicine. The role is a high-water mark for Agarwal, who is the product of an eclectic life’s journey, one that was guided by a wide array of influences and interests.
His parents hailed from Uttar Pradesh in northern India. His father graduated from the King George Medical College in the city of Lucknow and moved to southern India in 1959 to teach pathology at Kasturba Medical College at Mangalore University, a medical college in the coastal town of Mangalore.
Agarwal says his parents’ greatest gift to their three sons was education. “When I was young, my parents never wasted a moment in highlighting the value of great education and pushed us hard to make use of the best possible opportunities at school.”
Early Interests
Agarwal’s early education at St. Aloysius School, a Jesuit-run Catholic school in Mangalore, brought him into contact with classmates from a broad range of backgrounds and beliefs, some of whom he still calls friends. “My town was about 15 percent Catholic— the Portuguese and Italians who came in the 1500s to the coastal regions of southern India to spread Christianity settled there—and it has amazing diversity. There were about 60 students in my class, and we had Muslims, Hindus, Catholics. To this day I have a WhatsApp group of my former classmates, who remain highly engaged and active as a closely knit group of friends.”
Many of Agarwal’s overriding interests and passions began while he was a student at St. Aloysius. He became an avid cricket player and played ping-pong and basketball (“I was short so I was a good three-point shooter,” he says). He learned to play the Indian classical violin—in part inspired by his mother’s love of music—which contributed to his lifelong appreciation for classical music. Not surprisingly, Agarwal also showed an early aptitude for science.
Because his father was a pathology professor, Agarwal was essentially raised at the medical college. “We lived in campus housing growing up and my dad was the warden for the medical students’ residence hall. So I grew up hanging around medical students, even though they were much older than me.”
Given his upbringing, it seems inevitable that Agarwal would develop an interest in medicine, but he cites a specific event as the turning point that cemented his desire to become a physician. “My dad brought a specimen of a heart in a formalin-filled jar to my fourth-grade class. He explained to my class how the heart works and pumps blood, and I remember thinking, ‘Wow, I want to practice medicine.’ That was tremendous for me.”
 Agarwal at the University of Florida, where he worked from 1995-2003.
Agarwal at the University of Florida, where he worked from 1995-2003.
Making it to Medical School
Agarwal graduated St. Aloysius at the head of his class and entered Kasturba Medical College in 1980 after completing a two-year pre-university college (equivalent to 11th and 12th grade). While completing the Indian standard of six years of medical school, including a compulsory one-year rotating internship, he considered a number of specialties but ultimately settled on nephrology after encountering one of his earliest mentors in medicine. Agarwal decided to specialize in nephrology based on conversations with Brian Pereira, a nephrology fellow. Pereira argued that, “‘You can help patients through kidney transplantation and dialysis and their life is transformed. You can work in the intensive care unit managing acid-base, fluid, and electrolyte disorders and also take care of general medicine patients,’” according to Agarwal.
Another influential mentor during Agarwal’s residency training was the late Dr. Kirpal Singh Chugh, considered the father of nephrology in India. Agarwal remembers Chugh as being very patient-focused and having high expectations for his trainees. “Dr. Chugh was an exceptional teacher and mentor. He was very academically oriented. We’d be on rounds and he’d see a patient and say, ‘This is an interesting and unusual case presentation, we need to write this up and publish it so people can learn about it. Why don't you write this case?’ Then a week later he’d ask, ‘Where is this case report? I’d like to review it by tomorrow.’”
The Path to UAB
Agarwal completed three years of residency in internal medicine and three years of fellowship training in nephrology at the Postgraduate Institute of Medical Education and Research in Chandigarh. Then he encountered a roadblock that set him on a new path. “Academically at that time you couldn’t do much in terms of research in India, and my brother, who was already in the U.S., suggested that I do additional training in the U.S.” Agarwal says.
After passing the USMLE exams, Agarwal had a phone interview with the University of Minnesota. He was offered a fellowship position and was mentored there by Karl Nath, M.D., now at the Mayo Clinic in Rochester. “Karl was a most amazing and caring mentor. He took me into his lab, and I had never done basic research before, only clinical research. But it was a great experience—in those two years I was fortunate to have published three review articles and three first author papers.”
Agarwal spent three years as a nephology fellow at Minnesota and another year at the University of Florida in Gainesville, as a postdoctoral fellow/instructor in the lab of molecular biologist Harry Nick, Ph.D., where he met his wife, Lisa Curtis, Ph.D. The two were married in 2002.
Then in 2003 he was recruited to UAB by the former Director of Nephrology David Warnock, M.D. “It was the collaborations and the impressive medical school and health system that really excited me; I could see how quickly you could enable interactive collaborations here. Bruce Freeman, Ph.D., who was the vice chair for research of anesthesiology at the time, really influenced our decision to come. We initiated a collaboration even before I had moved to UAB, work that was subsequently published in the Proceedings of the National Academy of Sciences.”
2008-2021 Division Director, Nephrology • 2009-2014 Vice Chair of Research, Department of Medicine • 2011-2012 Interim Chair, Department of Medicine • 2013 Interim Senior Vice President for Medicine and Dean
• 2014-2022 Executive Vice Dean, Heersink School of Medicine 2023 Senior Vice President for Medicine and Dean
Putting Down Roots
The following year brought another landmark moment for Agarwal. “In 2004, I went to the federal courthouse in downtown Birmingham to get my U.S. citizenship conferred. There were about 160 of us from many different countries, and the judge said, ‘I want you all to know that just like you, my great-grandfather once sat in a crowd just like this.’”
Agarwal joined the Division of Nephrology as an associate professor and director of the Nephrology Research and Training Center. He was promoted to the rank of professor of Medicine in 2005 and went on to direct the NIH-funded O’Brien Center for Acute Kidney Injury Research, one of seven such centers in the nation. Agarwal’s research into the mechanisms of acute kidney injury has been continuously funded by the NIH for over 25 years.
In 2008, Agarwal succeeded Warnock as director of the Division of Nephrology, a position he held until 2021. In 2014, he was appointed to the newly created role of executive vice dean of the Heersink School of Medicine, where he worked closely with former Senior Vice President for Medicine and Dean Selwyn Vickers, M.D., FACS, and the dean’s leadership team. Upon Vickers’ departure, Agarwal was the natural choice for interim dean, having previously served in the role when the search that resulted in Vickers’ appointment as dean was underway.
In 2020, Agarwal became president of the American Society of Nephrology (ASN), the leading organization of nephrology health care professionals with more than 20,000 members representing more than 120 countries.
“I never thought in my wildest dreams when I first came here 30 years ago that I would be president of the ASN, the director of Nephrology, and now dean. I think one takeaway and lesson I have learned throughout my life has been knowing that I had to do my very best with the opportunities that came to me. I am forever grateful for all the opportunities that have been given to me.”
Now that he has been appointed dean, Agarwal continues to see patients at the Birmingham VA Medical Center. “I usually do inpatient consult service for nephrology, mainly in the intensive care unit. I really enjoy doing that so I hope to continue interacting with residents and fellows on the clinical service.”

Agarwal says he knows he’s in rare company as a person of Indian descent to become dean of a U.S. medical school. “This is a huge honor for someone who was trained in India and in the U.S. to become a medical school dean,” he says.
In addition to his professional duties, Agarwal is a father of two, son Alex (15) and daughter Megan (14). His many interests include golf and he is an avid supporter of the Alabama Symphony Orchestra, chairing the Physicians and Faculty for the Alabama Symphony Orchestra giving society. For his service he was given a commemorative conductor’s baton, which now hangs on his office wall.
The Road Ahead
As he plans for the future of the Heersink School of Medicine, Agarwal sees opportunities to address some of the most pressing health challenges facing our state and nation through the school’s tripartite mission in medical training, patient care, and biomedical research. In the medical training realm, Agarwal says his vision is for our school to “produce exceptional physicians prepared to provide compassionate care to all, reduce health disparities, advance treatments, and make discoveries.” He says this can be accomplished by enhancing access to and success in medical school for more students; enhancing pathways for medical students to be recruited to UAB residency programs; and identifying incentives for our graduates to practice in rural and underserved areas.
Among his key medical education goals are increasing the size of our medical school classes; expanding our graduate medical education (GME) programs to address the health care workforce needs of the state, particularly in primary care specialties and mental health; expanding integrated residency programs; and increasing scholarship funding for those with financial need.
5 Questions
with Dr. Agarwal
What are you currently reading?
Dan Berkowitz (chair of the Department of Anesthesiology and Perioperative Medicine) gave me an amazing book by Dacher Keltner that I’m reading right now called ‘Awe: The New Science of Everyday Wonder and How It Can Transform Your Life.’"
What is your favorite movie?
"I love action movies like the ‘Bourne Identity’ series, but a movie I’ve watched and rewatched is ‘Forrest Gump.’ I saw it in Minnesota on opening day in 1994 with another nephrology fellow and I said, ‘That movie is going to win all the Oscars this year.’"
What is your favorite restaurant?
“I love Blueprint on 3rd. They make a great burger with all these toppings and shoestring fries.”
Favorite golf course?
Pebble Beach in California
Do you have any pets?
“We have a six-year-old Goldendoodle named Lulu
Agarwal’s key priorities in clinical care include strengthening alignment and collaboration with the UAB Health System and its affiliate hospitals, as well as increasing capacity and improving access to care, especially in overcrowded units such as the Emergency Department, intensive care units, and operating rooms. “A recently completed clinical strategic planning effort will enable us to identify growth opportunities,” Agarwal says.
Strengthening rural hospitals by enhancing their capacities and expanding telehealth and hospital-at-home programs is also a key part of Agarwal’s vision. “A lot of what we’re doing with telemedicine is aimed at helping rural hospitals stay open,” says Agarwal. “Nationally, rural hospitals are shutting down at an alarming rate. Our telemedicine programs, through the leadership of Dr. Eric Wallace, have made a big difference in keeping the doors open at several rural hospitals here in Alabama.”
Agarwal also says the impact of digital health and artificial intelligence (AI) tools on health care is only beginning to be explored and will be transformational. “With new initiatives in artificial intelligence and digital health being led by our Marnix Heersink Institute for Biomedical Innovation, there are even more opportunities for innovation in health care delivery.”
In the research arena, Agarwal says the school’s four Research Focus Areas that were identified in 2022—Disruptive Technology Empowering Precision Health (D-TECH); Infection, Inflammation, Immunity, and Immunotherapy (I-4ward); Brain Health and Disease Across the Lifespan; and Health Equity—will serve as a roadmap to guide our future research recruitment and investment efforts.
Increasing NIH research funding and the school’s NIH funding ranking is an important part of Agarwal’s research vision. In the long-term, he says he wants the Heersink School of Medicine to achieve a top 20 ranking in NIH funding by 2030. He also seeks to expand and diversify the school's research portfolio with funding from agencies such as the Department of Defense, American Heart Association, American Cancer Society, and National Science Foundation. In addition, a UAB-wide initiative to establish a roadmap to reach $1 billion in total research expenditures announced this August seeks to increase funding from similar sources.
“I want us to continue to invest in our people, both by supporting currently funded projects and programs and by investing in recruitment. We want to recruit 100 new faculty investigators by 2030, and our recent past shows it can be done—we doubled our NIH funding and added 100 new investigators in the last eight-to-nine years.”
Agarwal says several construction projects that are currently underway will also aid recruitment. A new Biomedical Research and Psychology Building will house several research intensive departments from the Heersink School of Medicine, while renovations to the McCallum Basic Health Sciences Building, a longtime research hub on the school’s campus, will be completed in 2024.
Announced in December 2020, the Altec Styslinger Genomic Medicine and Data Sciences Building is part of the Heersink School of Medicine’s long-range plan to enhance research in genomic medicine and computational biology. The new building will encompass 145,000 square feet of new computational research, research support, office, administrative, and scientific collaboration and meeting spaces. Among Agarwal’s key priorities in research are addressing processes to reduce time to activation for clinical trials; investment in technology and instrumentation; enhancing career advancement pathways for trainees; and building upon collaboration with key partners, like Southern Research, a nonprofit scientific research organization, and the Birmingham VA Health Care System.
Agarwal says the Heersink School of Medicine also has a special responsibility to our state and region because of the school’s unique strengths and our state’s unique needs. “The economic impact we have, as a school and as a health system, puts us in a strong position to give back to our state and our region. That’s true at all levels—people depend on us for health care, for innovative treatments, and for training the next generation of physicians.”
Ultimately, Agarwal’s vision boils down to investing in people. “We have highly talented and committed faculty and staff as well as medical students, graduate students, residents, postdoctoral and clinical fellows, our nursing staff, our APPs (advanced practice providers)—our people at every level are high quality. They have a shared vision and goals that are aligned with the collaborative spirit of our institution, and that is our greatest strength.”
-By Jane Longshore