 Multimodal imaging in radiology spurs new perspectives on diagnosis and treatment.In the realm of technology, Moore’s Law states that computers double in power every two years. In radiology, which is driven by advances in imaging technology, there’s a similar principle at work. Every new piece of imaging equipment to hit the market offers faster results and higher-resolution radiological scans, as well as new possibilities in diagnosis and treatment.
Multimodal imaging in radiology spurs new perspectives on diagnosis and treatment.In the realm of technology, Moore’s Law states that computers double in power every two years. In radiology, which is driven by advances in imaging technology, there’s a similar principle at work. Every new piece of imaging equipment to hit the market offers faster results and higher-resolution radiological scans, as well as new possibilities in diagnosis and treatment.
Over the past few years at UAB, new imaging equipment and facilities, a new cyclotron particle accelerator to produce imaging agents, and advances in multimodal molecular imaging have made imaging more powerful than ever before.
“Each imaging agent can really be considered part of a toolbox,” says Suzanne Lapi, Ph.D., director of the UAB Radiochemistry Laboratory and Cyclotron Facility. “By combining tools, we’re not only seeing what something looks like, we can actually see the biology and the molecular pathways it’s using at the same time.”
People in the general public typically encounter radiology only for an occasional radiograph or magnetic resonance (MRI) examination, and regard the specialty as providing flat, static snapshots of their insides: a two-dimensional, black-and-white image of a broken wrist or a slipped disc, for example. But, as the field evolves, various imaging technologies—especially when used in combination—are providing more dynamic information for diagnostic purposes and pointing toward precision treatments for disease.
 Biomedical engineering student Retta El-Sayed (left) walks through the cyclotron vault with Cyclotron Facility Director Suzanne Lapi (right).“This approach utilizes not just MRI or CT or PET images, but takes different modalities and fuses them together,” says Cheri Canon, M.D., FACR, the Witten-Stanley Endowed Chair of Radiology. “This informs us not only of anatomy but also lets us study the physiology. And we have software that overlays images from two completely different types of equipment to give us collaborative information. In so many cases, there are now new ways to image disease or provide alternative therapies driven by advances in radiology.”
Biomedical engineering student Retta El-Sayed (left) walks through the cyclotron vault with Cyclotron Facility Director Suzanne Lapi (right).“This approach utilizes not just MRI or CT or PET images, but takes different modalities and fuses them together,” says Cheri Canon, M.D., FACR, the Witten-Stanley Endowed Chair of Radiology. “This informs us not only of anatomy but also lets us study the physiology. And we have software that overlays images from two completely different types of equipment to give us collaborative information. In so many cases, there are now new ways to image disease or provide alternative therapies driven by advances in radiology.”
From the Bottom Up
In 2013, a crane lowered a new cyclotron—used to create the radioactive isotopes needed for certain types of medical imaging—into the basement of the UAB Comprehensive Cancer Center’s Wallace Tumor Institute. In the five years since, this 60-ton piece of equipment has allowed UAB to start fine-tuning and combining new types of scans.
“Ours is one of the most sophisticated cyclotrons in an academic institution in the U.S.,” says Canon. And it’s located just a few steps from UAB’s Advanced Imaging Facility, which holds the latest and most advanced PET CT and PET MRI. Why does the proximity matter? Some of the radioactive materials being generated from scratch at UAB are active for mere minutes; they have to go straight from the cyclotron to being injected into a patient.
Each radiotracer used in medical scans must contain a radioactive element as a “beacon,” which is attached to the molecule that tells the material where in the body to go. In some cases, a physician wants to see the location of a tumor. In other cases, he or she may want to visualize the path blood takes through the heart, or see areas where oxygen or sugar are being metabolized differently than usual.
“The cyclotron lets us make radiotracers that are much more unique than what’s available commercially,” says Lapi. “We can develop markers of inflammation in the brain, for example, or visualize targets for different types of cancer. This gives the physician insight into how best to treat the patient.”
During a PET scan, radiotracers are swallowed, inhaled, or injected into the body. Then, depending on exactly what they’re designed to do, they accumulate in specific areas of the body. A PET scanner lets doctors visualize where the radiotracers end up. Brighter spots indicate that there are more radiotracers, because they bind to a desired target or undergo a desired chemical reaction.
On their own, PET scans may look fuzzy or imprecise—large blots of color showing areas of interest. By combining PET scans with simultaneous MRI or CT scans, which show the minute physical details of the body’s organs, physicians can better pinpoint exactly what they are looking at and where it is in the body.
Brain Power
According to Jonathan McConathy, M.D., Ph.D., director of UAB’s Advanced Imaging Facility, the cyclotron’s power combined with the strengths of the imaging facility not only give UAB the ability to better treat patients, by providing faster and more detailed imaging, but also help boost the school’s basic research efforts.
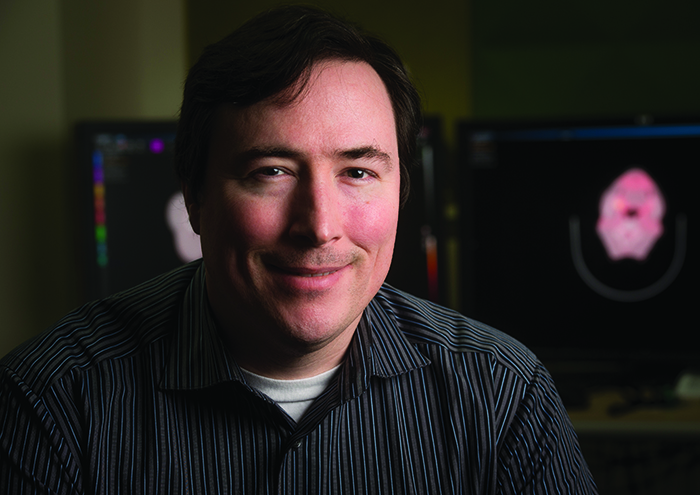 Jonathan McConathy directs UAB’s Advanced Imaging Facility. Photo by Steve Wood. “We’re using a lot of experimental radiotracers that aren’t being used in many other places,” he says. “And we’re working on developing brand new tracers here at UAB that will eventually be used in people.”
Jonathan McConathy directs UAB’s Advanced Imaging Facility. Photo by Steve Wood. “We’re using a lot of experimental radiotracers that aren’t being used in many other places,” he says. “And we’re working on developing brand new tracers here at UAB that will eventually be used in people.”
Among that basic research is the work that Lapi alluded to, which uses PET radiotracers to pinpoint inflammation in the brain. Studies have suggested that levels and locations of brain inflammation are critical to the progression of Parkinson’s disease. UAB researchers are in the early stages of testing whether visualizing brain inflammation using PET scans—with radiotracers highlighting areas of inflammation—can help diagnose or track the progression of Parkinson’s disease.
In another project, UAB researchers are combining MRI and PET scans to detect levels of certain proteins in the brains of people with Alzheimer’s disease. In this case, the PET radiotracers are designed to seek out amyloid or tau proteins, which are known to accumulate abnormally in Alzheimer’s disease. Doctors hope the multimodal images will eventually lead to ways to diagnose Alzheimer’s earlier.
“This research is really critical if you’re doing studies with patients who you think might have Alzheimer’s but are very early in the disease progression or don’t have typical symptoms,” says McConathy. “Often these people are misdiagnosed, but these scans help us be much more certain of their diagnosis.”
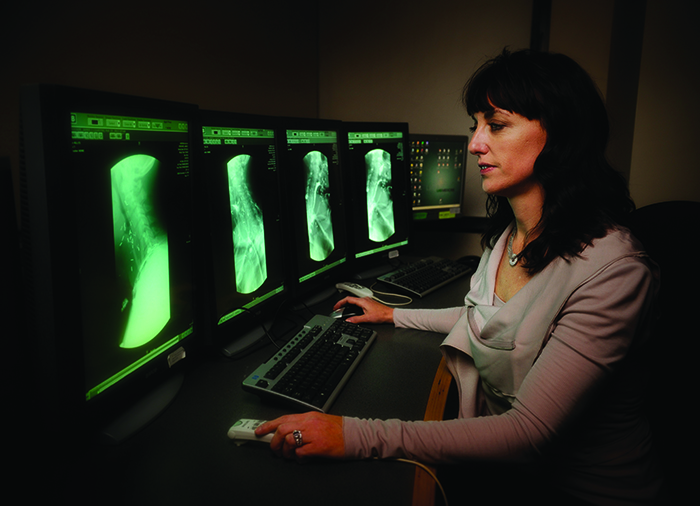
While those types of scans can help diagnose Alzheimer’s and Parkinson’s, they don’t point toward treatments yet. However, other brain scans are already helping guide surgeries. Philip Chapman, M.D., chief of neuroradiology, says UAB neurosurgeons are relying on two types of scans—functional MRI or fMRI, and diffusion tensor imaging or DTI—to map out the brains of brain cancer and epilepsy patients before their surgeries.
In an fMRI, a neuroradiologist might ask a patient to move his or her hand or fingers. The fMRI scan then detects which areas of the brain have increased blood flow, indicating activity. This lets the neuroradiologist pinpoint exactly where the brain’s motor, or movement, areas are. Similarly, an fMRI conducted while a patient is reading or talking might point toward the language area of the brain.
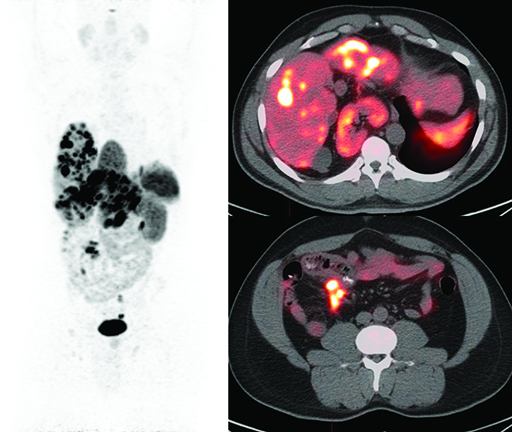 The whole-body PET image (left) of a patient with a neuroendocrine tumor that has spread to the liver shows the tracer Gallium-68-DOTATATE binding to the tumor as dark spots, while the fused PET/CT images of the liver (top right) and lower abdomen (bottom right) show binding as white and orange spots.In conjunction with fMRI, performing a DTI scan—which tracks the movement of water—lets clinicians see the location of tracts of white matter in the brain. Disrupting these superhighways of information during a surgery can interrupt connections among areas of the brain involved in such vital functions as vision, movement, and reasoning.
The whole-body PET image (left) of a patient with a neuroendocrine tumor that has spread to the liver shows the tracer Gallium-68-DOTATATE binding to the tumor as dark spots, while the fused PET/CT images of the liver (top right) and lower abdomen (bottom right) show binding as white and orange spots.In conjunction with fMRI, performing a DTI scan—which tracks the movement of water—lets clinicians see the location of tracts of white matter in the brain. Disrupting these superhighways of information during a surgery can interrupt connections among areas of the brain involved in such vital functions as vision, movement, and reasoning.
“If you have a brain tumor that’s pushed normal language or motor structures of the brain out of place, it’s important to know where they’re being displaced to,” says Chapman. “This lets the surgeon plan ahead of time how to navigate around those important areas.” With these techniques, surgeons removing a brain tumor or an epileptic lesion can better avoid long-term damage to a patient’s ability to walk or talk.
Chapman and other UAB neuroradiologists have also recently ramped up their use of CT perfusion scans in patients admitted to the hospital after a stroke. Traditional CT scans of the brain can reveal where a stroke has already happened. CT perfusion, which images the areas of the brain that have blood supply, can point clinicians toward areas of the brain that are at risk of stroke.
“This tells us who might have additional strokes in the hours or days after an initial stroke if they don’t get treatment,” says Chapman. “It’s incredibly useful to be able to target treatment, and is becoming more of a standard here at UAB.”
Heart of the Matter
It is not only the brain that is being visualized more clearly than ever before; physicians can also see finer details of the heart, which helps them treat heart disease with greater precision.
“The scanners we have now are faster than ever before, so we can scan the heart in the time span of one single breath hold—three or four seconds,” says Satinder Singh, M.D., chief of cardiopulmonary radiology and director of cardiac CT at UAB. “The quality of the images is much better and the radiation dose is much lower than in the past.”
To diagnose coronary artery disease—the narrowing of the arteries that carry blood to the heart—doctors often rely on stress tests, which gauge how the heart responds to exercise or other stressors. But in some cases, a patient’s symptoms don’t match the results of their stress test and further testing is required.
In the past, calculating the severity of the narrowing of the heart’s arteries involved inserting a thin wire and catheter into the arteries from the groin. Now, UAB radiologists are using CT scans to not only visualize the narrowing of arteries but also to look at the vessel walls to find high-risk plaques noninvasively.
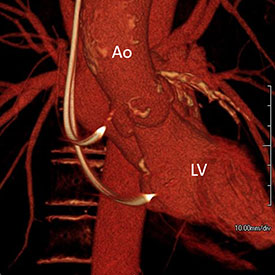
They are also turning to CT scans to help plan complex valve replacements. While valves are traditionally replaced in an open-heart surgery, physicians have recently begun turning to a less-invasive procedure for patients who aren’t good candidates for surgery. In a transcatheter aortic valve replacement (TAVR), a hollow tube is guided through a patient’s arteries—from his/her leg or arm—to the heart. Once in place, the tube is used to deploy a replacement valve.
“There’s a lot of critical information the surgeon needs to deploy the valve correctly and avoid complications,” says Singh. CT scans ahead of surgery can help determine the best access site, size of the valve needed, and the exact angle for valve deployment.
Singh and his colleagues have also started using CT scans after valve replacements to screen patients for complications. In a small segment of valve replacements, the replaced valve develops thrombus—a blood clot—and patients who have this complication often don’t show symptoms. Only a CT scan can confidently detect the valve thrombus, which can then be easily treated with blood thinners.
“We now have about a dozen cases where patients had no symptoms but came in for their follow-up appointments. They were found to have increased pressures across the valve on heart ultrasound, and the CT scan was able to detect thrombus,” says Singh. “So we’re catching these patients much earlier and treating them early.”
Scans to Treat
Just as cardiac radiologists are using CT scans to guide the catheter tubes used in TAVR procedures, interventional radiologists at UAB are guiding catheters through arteries to treat conditions elsewhere in the body.
“There’s a general interest in moving treatment from invasive to minimally invasive whenever possible,” says Ahmed Kamel, M.D., M.Sc., Ph.D., chief of interventional radiology. The entire field of interventional radiology, in fact, revolves around using imaging to precisely guide treatments. Chemotherapy, for instance, can be loaded on small diameter beads and directly injected into a tumor using X-rays to guide the chemotherapy injection to the spot of the cancer.
 Cheri Canon is the chair of the Department of Radiology.A procedure called fibroid embolization to treat uterine fibroids offers women a less invasive alternative to total hysterectomy to remove the uterus. Interventional radiologists guide very small beads into the arteries of the uterus and block the blood supply to fibroids. “Women get significant relief of their symptoms but are back to work very quickly and with no incisions in their pelvis,” Kamel says.
Cheri Canon is the chair of the Department of Radiology.A procedure called fibroid embolization to treat uterine fibroids offers women a less invasive alternative to total hysterectomy to remove the uterus. Interventional radiologists guide very small beads into the arteries of the uterus and block the blood supply to fibroids. “Women get significant relief of their symptoms but are back to work very quickly and with no incisions in their pelvis,” Kamel says.
More recently, interventional radiologists have begun performing prostate artery embolizations, in which very small beads are injected into the prostate using image guidance. The beads block blood flow to the prostate, eventually shrinking it. The procedure—which UAB is the first to offer in the state—is used to treat benign prostate hyperplasia, a condition that is common in older men and can cause frequent or difficult urination.
As imaging techniques continue to improve and clinicians find new ways to use and combine scans, radiologists expect that their expertise will only become more critical to diagnosis and treatment.
“Imaging is really the hub of diagnosis across many diseases,” says Canon. “And it’s also becoming the prototype for precision medicine.” According to Canon, imaging increasingly helps physicians not only guide the location of a treatment, but select treatments, predict whether a treatment will work, or determine whether an existing course of treatment is currently working. As new radiotracers allow the visualization of particular molecules, for instance, physicians may be able to match molecular markers in a patient’s body to drugs that target those markers.
“Health care is rapidly changing, and everyone has to do more with less,” says Canon. “Imaging is specifically challenging because our imaging modalities are so expensive, but UAB has done a fantastic job of keeping on the cutting-edge of radiology, and that has really set us apart and allowed for increased precision in disease diagnosis for our patients.”
By Sarah Williams